- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
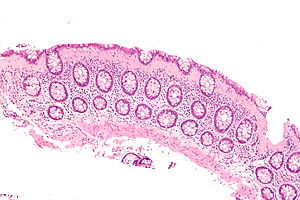
Microscopic colitis patients at an increased risk of premature death finds study
Sweden: Microscopic colitis patients are at an increased risk of premature death. This could be due to gastrointestinal, cardiovascular, and infectious conditions. The population-based study demonstrated that people having microscopic colitis for more than 10 years are 20% more likely to die compared to those without the disorder.
These are findings from a recent study presented at the 2019 Digestive Disease Week (abstract 513).
Microscopic colitis is a chronic inflammatory disorder of the colon primarily affecting postmenopausal women. It is a condition characterized by inflammation of the large intestine (colon) causing persistent watery diarrhoea.
Hamed Khalili, Massachusetts General Hospital in Boston, and colleagues examined mortality in 14,520 patients with microscopic colitis from a nationwide GI-specific pathology database in Sweden.
Each case was matched with five individuals from a pool of 69,489 people in the Swedish Population Register. Researchers also used the Swedish Sibling Registry to compare deaths among the cases with those of their unaffected siblings. More than 70% of the cases were female, diagnosed at a mean of 60 years of age and followed for a mean of eight years. Aside from celiac disease, baseline comorbidities were similar in cases and controls.
The follow-up time was calculated from the time of diagnosis to death, emigration or end of the study. Analyses were adjusted for other concurrent GI diseases.
Also Read: Use of menopausal hormone therapy linked to microscopic colitis
Key findings include:
- Celiac disease was noted at baseline in 5.4% of patients with microscopic colitis but only 0.2% of the general population.
- The age-adjusted model for this nationwide cohort revealed a 20% relative increase in the risk of death from all causes in patients with microscopic colitis.
- The difference reflected an approximate 3% increase in absolute risk at 20 years, with significant increases seen in deaths related to cardiovascular, GI and infectious conditions, but not cancer.
- Gastrointestinal- and infection-related deaths were about twofold higher than the general population comparators. The difference appeared to be largely attributable to an increase in deaths among patients with collagenous colitis, whose risk was increased by 30%.
- Cause-specific mortality per 1,000 person-years was 23 for the general population, 27.1 for microscopic colitis, 32.6 for collagenous colitis and 24.6 for lymphocytic colitis.
- The adjusted hazard ratios were 1.2 for microscopic colitis, 1.3 for collagenous colitis and 1.1 for lymphocytic colitis.
- The absolute increase in deaths over time for patients with microscopic colitis versus controls was 1.9% at five years, 1.5% at 10 years, 2.9% at 15 years and 2.8% at 20 years.
- The risk of death increased with longer duration of disease or longer duration of follow-up so that individuals who had microscopic colitis for more than 10 years had about a 30% increase in the risk of death.
- The sensitivity analysis comparing patients with unaffected siblings showed an adjusted hazard ratio of 1.2, identical to the primary analysis.
“We had a relatively short follow-up [mean, eight years], but we saw that a longer duration of the disease was actually associated with increased risk of all-cause death. Also, data on important lifestyle factors, such as body mass index [BMI] were not available, but lean BMI is more common among these patients than those with high BMI. We think, therefore, that adjusting for BMI would have actually strengthened our observed association,” said Dr Khalili. “We also did not have detailed endoscopic and clinical data across all patients, but a prior validation study showed that our method of identifying microscopic colitis has high positive predictive value for symptomatic disease”

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd