- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
World Report on Fertility Treatments Reveals High Use of ICSI
The editor-in-chief of one of the world's leading reproductive medicine journals has attacked the rising use of intracytoplasmic sperm injection (ICSI) for the treatment of infertility, following publication of the latest world report on assisted reproductive technologies (ART).
The report in Human Reproduction shows that while ICSI use has levelled off in some regions, its use is approaching 100% of assisted reproduction cycles in the Middle East and a few countries in other regions, despite the fact that ICSI was developed for the treatment of male infertility, which is a factor in around 40% of couples seeking fertility treatment. The world report covers the years 2008, 2009 and 2010 - the years for which the most recent data are available.
In an editorial entitled "Santa Claus in the fertility clinic", to accompany the world report by the International Committee for Monitoring Assisted Reproductive Technologies (ICMART), Professor Hans Evers highlights the fact that in 2010 there were 220,000 in vitro fertilisation (IVF) treatments, but there were more than 455,000 ICSI treatments in the world. There was 1.4 times as much ICSI than IVF in Asia, twice as much in sub-Saharan Africa, just over twice as much in Europe, 2.7 times as much in North America, more than six times as much in Latin America and more than 60 times as much in the Middle East.
He writes that doctors are guilty of over-estimating the effect of ICSI. "The majority of the patients who will get pregnant with intracytoplasmic sperm injection (ICSI) will also do so with IVF". Studies have shown that ICSI results in fewer live births than IVF when used for couples where male infertility is not the problem. "Intending to improve their patients' pregnancy probability by preventing fertilization failure, well-meaning doctors actually decrease their chances. This has to stop. We have pledged to do no harm," he writes.
Prof Evers says doctors will serve their patients best by making decisions based on the evidence, "not by playing Santa Claus and doling out nicely wrapped presents of unnecessary, ineffective and costly care".
The authors of the ICMART report say that the reasons behind the high use of ICSI are not fully understood and are beyond the scope of their report. They write: "Investigating why ICSI is a preferred fertilization technique in a number of countries, particularly in Latin America and the Middle East, is warranted."
The report includes data from nearly 2,500 ART clinics from between 58 and 61 countries in the years 2008, 2009 and 2010, and it is the first time the report has included all regions of the world, with the first submissions of data from some sub-Saharan African countries.
During the three years, more than 4,461,300 ART cycles were carried out, resulting in an estimated 1,144,858 babies born around the world. This represents a 9.5% increase in the number of cycles over the three years and a 9.1 increase in babies born.
The report shows wide variation in the use of ART between countries. Globally, ART use remained fairly constant, with 436 cycles per million of the population in 2008 and 474 cycles per million in 2010. However, ART use ranged from 4,775 cycles per million in Israel (which had consistently the highest levels of access over the three years) to just eight cycles per million in the Dominican Republic in 2010. In the same year there were almost 2,500 cycles per million in Australia and New Zealand, more than 900 per million in Europe, 570 cycles per million in North America, 150 cycles per million in Latin America and nearly 90 cycles per million in sub-Saharan Africa. The authors of the report write that the global figure for the use of ART "conservatively represents less than 20% of the demand for ART treatment being met".
The safety of ART improved, with an increase in the number of single embryos transferred per cycle. This increased from 25.7% in 2008 to 30% in 2010, while the average number of embryos transferred fell from 2.1 to 1.9 and the rates of twin and triplet births also fell. However, there were wide regional variations: in Australia and New Zealand 8.2% of ART births were twins, but 30% were twins in the Middle East. The practice of freezing embryos and then thawing them and transferring them to women's wombs (known as frozen embryo transfer or FET) also increased by 27.6% between 2008 and 2010; FET cycles had approximately half the multiple birth rate when compared with fresh embryo transfers, namely 13% (2008), 11.9% (2009) and 12% (2010), with just 0.6% triplet births in all three years.
The first author of the ICMART report, Professor Silke Dyer, a senior specialist in reproductive medicine in the Department of Obstetrics and Gynaecology, at Groote Schuur Hospital and the University of Cape Town, South Africa, said: "The move towards single embryo transfer (SET) and thus towards greater safety and better outcome for ART is a significant finding. Very importantly, however, SET is not a stand-alone practice or finding, but closely related to the cost patients pay for treatment, and to utilisation rates and the use of FET. Supportive funding of ART, either through public or third party funding [4], increases utilisation through the provision of more affordable ART treatment, and at the same time encourages SET, which in turn allows for the freezing of excess embryos. This means patients and doctors are under less pressure to maximise the immediate chance of pregnancy by transferring more than one embryo, which comes with the risk of multiple pregnancy.
"We must acknowledge that this approach carries additional cost. However, given that the optimal outcome of fertility treatment is a healthy single live birth, supportive funding meets the dual goals of equitable access to treatment and safer outcomes for ART-conceived children and mothers. The global multiple birth rate of 21.5% in 2010 is still too high, and policy and practice should seek to reduce the multiple birth rates.
"Through this three-year report, as well as our previous reports, we contribute to a global understanding of the role of scientific data, and how these data can and should inform sound policy-making."
[1] "International Committee for Monitoring Assisted Reproductive Technologies world report on assisted reproductive technologies: 2008-2009-2010", by S.Dyer et al. Human Reproduction journal. doi:10.1093/humrep/dew082.
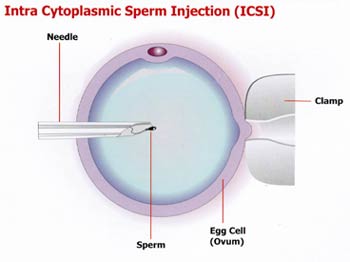
[2] ICSI is a technique in which a single sperm is injected into the centre of a woman's egg. It is designed to be used in situations where there are very few good quality sperm available for conventional in vitro fertilisation (IVF) techniques.
[3] "Santa Claus in the fertility clinic", by J.L.H. (Hans) Evers. Human Reproduction journal. doi:10.1093/humrep/dew092.
[4] Third party funding covers funding by neither the supplier (hospital or unit through their internal funds) nor the patient; the third party could be a medical aid or insurance scheme, or a government fund or other funding models.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd