- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Women with PCOS have double the risk of non-alcoholic fatty liver disease
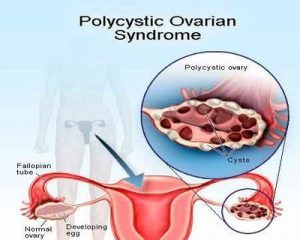
Polycystic ovary syndrome (PCOS) affects 10 percent of all women and is associated with irregular periods, impaired fertility, male-pattern body hair growth and acne. As a number of women who have PCOS have higher levels of male hormones they are less sensitive to insulin and are overweight or obese.Given the obesity link to both PCOS and non-alcoholic fatty liver disease, Scientists at the University of Birmingham conducted a study to explore the relationship between PCOS and non-alcoholic fatty liver disease both in terms of prevalence and cause.They have found that increased male hormones result in women with polycystic ovaries having a two-fold increased risk of developing the non-alcoholic fatty liver disease (NAFLD).The study has been published in PLOS Medicine.
The non-alcoholic fatty liver disease is an umbrella term for a range of liver conditions affecting people who drink little or no alcohol and is a major cause of liver disease worldwide. The main characteristic of the non-alcoholic fatty liver disease is too much fat stored in liver cells. Experts don't know exactly why some people accumulate fat in the liver while others do not, a however non-alcoholic fatty liver disease has been linked to obesity.
Now scientists have discovered that women with PCOS are two to three times more likely to develop the non-alcoholic fatty liver disease than women without PCOS. And, importantly, the research found that women with both PCOS and a high testosterone level are at an increased risk of non-alcoholic fatty liver disease regardless of their weight.
In the largest study of its kind, the scientists compare the health records of 63,000 women with PCOS to 120,000 women of similar age, body weight and background. They also specifically looked at two cohorts of women with PCOS and women with high levels of testosterone.
Dr Krish Nirantharakumar, of the University of Birmingham's Institute of Applied Health, said: "We observed a two-fold increased risk of fatty liver disease in women with PCOS and male hormone excess.
"Looking at the levels of the major male hormone testosterone, we found that having a high testosterone level increased the risk of fatty liver disease significantly, even in women who were of a normal healthy weight."
Professor Wiebke Arlt, Director of the University of Birmingham's Institute of Metabolism and Systems Research, said: "Our research has highlighted significant and previously unknown health risks in women with PCOS and increased male hormone levels.
"Our findings suggest that regular screening for the fatty liver disease should be considered in these women, to make sure the disease is caught early."
"Our research shows that PCOS does not only affect fertility but also comes with significantly increased rates of metabolic complications."
"This means that women with PCOS need integrated health care throughout their life and not only when planning a pregnancy."
For more details click on the link: https://doi.org/10.1371/journal.pmed.1002542
Dr Krish Nirantharakumarfatty liver diseasefertilityjournal PLoS Medicinemetabolic complicationsmetabolismNAFLDNon-alcoholic fatty liver diseasePCOSPLOS Medicinepolycystic ovary syndrome
Source : With inputs Eureka AlertNext Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd