- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Why losartan is effective in Marfan Syndrome?
Losartan, a common blood-pressure-lowering medication, is routinely used prophylactically by Marfan patients to help prevent or delay aortic root disease and is one of the two medications recommended by current guidelines. A new study conducted by Dr.Pascal-Nicolas Bernatchez, of the Department of Anesthesiology, Pharmacology and Therapeutics, University of British Columbia, Vancouver it has been confirmed that Losartan is effective in Marfan's Syndrome but its mode of action may be different from one that was previously thought. The researchers report in American Journal of Pathology that activation of endothelial function and protective endothelial nitric oxide release appear to be key to losartan's anti-aortic root remodeling activities.
Losartan, a common blood-pressure-lowering medication, is routinely used prophylactically by Marfan patients to help prevent or delay aortic root disease. "Our team has identified a possible new direction for the management of Marfan patients. Contrary to most preconceptions, reducing blood pressure and heart rate does not attenuate aortic root widening in Marfan mice. Instead, activation of endothelial function and protective endothelial nitric oxide release appear to be key to losartan's anti-aortic root remodeling activities. This was completely unexpected," explained Pascal-Nicolas Bernatchez, PhD, of the Department of Anesthesiology, Pharmacology and Therapeutics, University of British Columbia, Vancouver. "From a patient outcome perspective, our data support the concept that focusing on blood pressure lowering and cardiac hemodynamics in Marfan syndrome might be of low therapeutic value, whereas focusing on gains in endothelial function might be preferable."
Losartan is recommended for Marfan patients due to its unique anti-remodeling properties, which other antihypertensive agents, such as angiotensin converting enzyme inhibitors (ACEi), lack. (Vascular remodeling refers to changes in the structure of blood vessels, such as increased wall thickness or lumen diameter.) In Marfan syndrome the pathological changes in the aortic root are thought to be related to angiotensin II receptor 1 (ART1) signaling and the anti-remodelling effects of losartan mediated by blocking ART1 signaling and downstream transforming growth factor-beta. The current study proposes a more complex view of this pathway.
In collaboration with Investigators from the British Columbia Children's Hospital Research Institute, the team used genetically altered mice that display many of the features of Marfan syndrome and bred them with hypotensive and bradycardic mice with blunted ATR1 expression. To their surprise, the progeny developed aortic root disease aggressively and remained fully responsive to losartan, indicating a possible "off target" effect that results in increased anti-remodelling nitric oxide release.
"This could explain why losartan is considered a wonder drug, since it has the unique ability to activate protective endothelial function in disease settings, something aerobic exercise is also known to do. Therefore, we may have documented a novel way to activate endothelial function in a therapeutically-meaningful manner and characterized differences between blood pressure regulation and nitric oxide-dependent endothelial function, noted Dr. Bernatchez.
The investigators propose that other antihypertensive agents do not share losartan's ability to activate endothelial function and may explain why they are not beneficial for Marfan syndrome. Titrating the dose of losartan according to the effect on endothelial function may optimize treatment in the future, whereas new therapies may be developed to focus on the anti-remodelling properties of endothelial function.
"Our findings stress the importance of activating protective endothelial function and nitric oxide release during losartan treatment, a concept supported by the work of other member of our research group. Endothelial function activation could be the basis for improved Marfan patient management," commented Dr. Bernatchez.
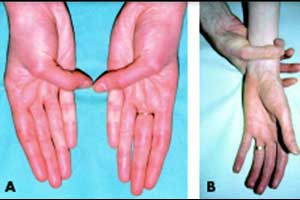
Marfan syndrome is an autosomal dominant connective tissue disorder that occurs in 1 in 5,000 to 10,000 individuals. Affected individuals have mutations in the fibrillin 1 gene and these interfere with the proper formation and stabilization of elastic fibers in the walls of blood vessels and other tissues. The most serious manifestation of Marfan syndrome is progressive aortic root dilation with increased risk of mitral valve prolapse and aortic aneurysm. Other problems may arise in the lungs, eyes, bones, and covering of the spinal cord. Individuals diagnosed with Marfan syndrome are often tall and thin, with long arms, legs, fingers, and toes.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd