- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
WHO guidelines on Chronic Hepatitis B
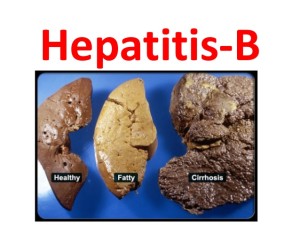
Two billion individuals in the world have evidence of past or present hepatitis B, chronically infected with hepatitis B. Many of these people appear healthy but can spread the virus to others.Hepatitis B infection is transmitted through sexual contact, contact with contaminated blood (for example, through shared needles used for illicit, intravenous drugs), and from mother to child. Hepatitis B is not spread through food, water, or casual contact. Serologic (blood) markers specifically for hepatitis B virus are used to diagnose hepatitis B viral infection. The blood tests can also identify the stage of the infection (past or present) and people who are at highest risk for complications.Injury to the liver by hepatitis B virus is caused by the body's immune response as the body attempts to eliminate the virus.
Hepatitis B is preventable through vaccination. All children should receive the vaccine. In addition, adults at high risk for hepatitis B should be vaccinated. Unvaccinated people who are exposed to hepatitis B should be evaluated by a physician to determine if they need specific immune globulin
World Health Organization (WHO) in 2015 published guidelines for the 'Prevention, Care and Treatment of persons with chronic hepatitis B infection.' Following are the new recommendations:
Non-invasive Assessment of Liver Disease Stage at Baseline and during Follow up
Aspartate aminotransferase (AST)-to-platelet ratio index (APRI) is recommended as the preferred non-invasive test (NIT) to assess for the presence of cirrhosis (APRI score >2 in adults) in resource-limited settings. Transient elastography (e.g., FibroScan) or FibroTest may be the preferred NITs in settings where they are available and cost is not a major constraint. (Conditional recommendation)
Who to Treat and Who Not to Treat in Persons with Chronic Hepatitis B
Who to Treat
As a priority, all adults, adolescents and children with chronic hepatitis B (CHB) and clinical evidence of compensated or decompensated cirrhosis (or cirrhosis based on APRI score >2 in adults) should be treated, regardless of alanine aminotransferase (ALT) levels, hepatitis B e antigen (HBeAg) status or hepatitis B virus (HBV) deoxyribonucleic acid (DNA) levels. (Strong recommendation)
Treatment is recommended for adults with CHB who do not have clinical evidence of cirrhosis (or based on APRI score ≤2 in adults), but are aged more than 30 years (in particular), and have persistently abnormal ALT levels and evidence of high-level HBV replication (HBV DNA >20,000 IU/mL), regardless of HBeAg status. (Strong recommendation)
Where HBV DNA testing is not available: Treatment may be considered based on persistently abnormal ALT levels alone, regardless of HBeAg status. (Conditional recommendation)
Existing Recommendation for HBV/Human Immunodeficiency Virus (HIV)-Coinfected Persons
In HBV/HIV-coinfected individuals, antiretroviral therapy (ART) should be initiated in all those with evidence of severe chronic liver disease, regardless of CD4 count; and in all those with a CD4 count ≤500 cells/mm3, regardless of stage of liver disease. (Strong recommendation)
Who Not to Treat But Continue to Monitor
Antiviral therapy is not recommended and can be deferred in persons without clinical evidence of cirrhosis (or based on APRI score ≤2 in adults), and with persistently normal ALT levels low levels of HBV DNA replication (HBV DNA 20,000 IU/mL but persistently normal ALT levels
HBeAg-negative persons without cirrhosis aged 30 years or less, with HBV DNA levels that fluctuate between 2000 and 20,000 IU/mL, or who have intermittently abnormal ALT levels
Where HBV DNA testing is not available: Persons without cirrhosis aged 30 years or less, with persistently normal ALT levels, regardless of HBeAg status
First-Line Antiviral Therapies for Chronic Hepatitis B
In all adults, adolescents and children aged 12 years or older in whom antiviral therapy is indicated, the nucleos(t)ide analogues (NAs) which have a high barrier to drug resistance (tenofovir or entecavir) are recommended. Entecavir is recommended in children aged 2–11 years. (Strong recommendation)
NAs with a low barrier to resistance (lamivudine, adefovir or telbivudine) can lead to drug resistance and are not recommended. (Strong recommendation)
Existing Recommendation for HBV/HIV-Coinfected Persons
In HBV/HIV-coinfected adults, adolescents and children aged 3 years or older, tenofovir + lamivudine (or emtricitabine) + efavirenz as a fixed-dose combination is recommended as the preferred option to initiate ART. (Strong recommendation)
Second-Line Antiviral Therapies for the Management of Treatment Failure
In persons with confirmed or suspected antiviral resistance (i.e., history of prior exposure or primary non-response) to lamivudine, entecavir, adefovir or telbivudine, a switch to tenofovir is recommended. (Strong recommendation)
When to Stop Treatment
Lifelong NA Therapy
All persons with cirrhosis based on clinical evidence (or APRI score >2 in adults) require lifelong treatment with NAs, and should not discontinue antiviral therapy because of the risk of reactivation, which can cause severe acute-on-chronic liver injury. (Strong recommendation)
Discontinuation
Discontinuation of NA therapy may be considered exceptionally in:
Persons without clinical evidence of cirrhosis (or based on APRI score ≤2 in adults)
And who can be followed carefully long term for reactivation
And if there is evidence of HBeAg loss and seroconversion to anti-HBe (in persons initially HBeAg positive) and after completion of at least one additional year of treatment
And in association with persistently normal ALT levels and persistently undetectable HBV DNA levels (where HBV DNA testing is available)
Where HBV DNA testing is not available: Discontinuation of NA therapy may be considered in persons who have evidence of persistent hepatitis B surface antigen (HBsAg) loss and after completion of at least one additional year of treatment, regardless of prior HBeAg status. (Conditional recommendation)
Retreatment
Relapse may occur after stopping therapy with NAs. Retreatment is recommended if there are consistent signs of reactivation (HBsAg or HBeAg becomes positive, ALT levels increase, or HBV DNA becomes detectable again) (where HBV DNA testing is available). (Strong recommendation)
Monitoring
Monitoring for Disease Progression and Treatment Response in Persons with CHB prior to, during and Post-treatment
It is recommended that the following be monitored at least annually:
- ALT level (and AST for APRI), HBsAg, HBeAg, and HBV DNA levels (where HBV DNA testing is available)
- Non-invasive tests (APRI score or FibroScan) to assess for the presence of cirrhosis, in those without cirrhosis at baseline
- If on treatment, adherence should be monitored regularly and at each visit. (Strong recommendation)
More Frequent Monitoring
In persons who do not yet meet the criteria for antiviral therapy: More frequent monitoring for disease progression may be indicated in: persons who have intermittently abnormal ALT levels or HBV DNA levels that fluctuate between 2000 IU/mL and 20,000 IU/mL (where HBV DNA testing is available), and in HIV-coinfected persons. (Conditional recommendation)
In persons on treatment or following treatment discontinuation: More frequent on-treatment monitoring (at least every 3 months for the first year) is indicated in: persons with more advanced disease (compensated or decompensated cirrhosis); during the first year of treatment to assess treatment response and adherence; where treatment adherence is a concern; in HIV-coinfected persons; and in persons after discontinuation of treatment. (Conditional recommendation)
Monitoring for Tenofovir and Entecavir Toxicity
Measurement of baseline renal function and assessment of baseline risk for renal dysfunction should be considered in all persons prior to initiation of antiviral therapy.
Renal function should be monitored annually in persons on long-term tenofovir or entecavir therapy, and growth monitored carefully in children. (Conditional recommendation)
Monitoring for Hepatocellular Carcinoma
Routine surveillance for hepatocellular carcinoma (HCC) with abdominal ultrasound and alpha-fetoprotein testing every six months is recommended for:
- Persons with cirrhosis, regardless of age or other risk factors (Strong recommendation, low quality of evidence)
- Persons with a family history of HCC (Strong recommendation, low quality of evidence)
- Persons aged over 40 years (lower age may apply according to regional incidence of HCC), without clinical evidence of cirrhosis (or based on APRI score ≤2), and with HBV DNA level >2000 IU/mL (where HBV DNA testing is available). (Conditional recommendation)
Prevention
Infant and Neonatal Hepatitis B Vaccination
Existing Recommendations in Infants and Neonates
All infants should receive their first dose of hepatitis B vaccine as soon as possible after birth, preferably within 24 hours, followed by two or three doses.
Prevention of Mother-to-Child HBV Transmission Using Antiviral Therapy
In HBV-monoinfected pregnant women, the indications for treatment are the same as for other adults, and tenofovir is recommended. No recommendation was made on the routine use of antiviral therapy to prevent mother-to-child HBV transmission.
Existing Recommendations in HIV-Infected Pregnant and Breastfeeding Women
In HIV-infected pregnant and breastfeeding women (including pregnant women in the first trimester of pregnancy and women of childbearing age), a once-daily fixed-dose combination of tenofovir + lamivudine (or emtricitabine) + efavirenz is recommended as first-line ART. This recommendation applies both to lifelong treatment and to ART initiated for prevention of mother-to-child transmission (PMTCT) and then stopped. (Strong recommendation)
Next Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd