- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Vanishing metatarsal: a rare manifestation of primary hyperparathyroidism

The case of Vanishing metatarsal: a rare manifestation of primary hyperparathyroidism has been published in BMJ Case Reports.
A 31-year-old woman presented with a history of bone pains, difficulty in walking and painless swelling of the left foot for the last 1 year (figure 1). X-ray of the left foot showed multiple lytic lesions in metatarsal bones and the absence of proximal half of shaft of second metatarsal. Biochemistry results revealed corrected serum calcium 11.2 mg/dL, phosphate 2.0 mg/dL, alkaline phosphatase 1049 IU/mL, intact parathyroid hormone (iPTH) 2543 pg/mL, 25-hydroxyvitamin D 16.2 ng/mL, and serum creatinine 0.6 mg/dL. She had no history of pancreatitis or evidence of renal/gall stone disease. The skeletal survey showed multiple osteitis fibrosa cystica (OFC) lesions, pathological fracture of shaft of the left femur and salt and pepper appearance of the skull (figure 2a, b, c). Sestamibi scan revealed right inferior parathyroid adenoma measuring 3.0×2.9×2.2 cm. Based on the above findings, a diagnosis of primary hyperparathyroidism (PHPT) was made and she underwent parathyroid adenectomy. Tumour weighed 4 g and histopathology was consistent with clear cell parathyroid adenoma.
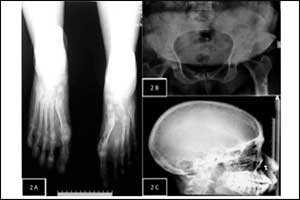 Image Source: Figure 2
Image Source: Figure 2(A) X–ray of both foot showing generalised demineralization of foot bones, multiple lytic lesions (brown tumours) and apparent disappearance of proximal half of second metatarsal of the left foot. (B) X–ray of pelvis showing ill-defined lucencies in bilateral iliac, pubic and ischial bones, and pathological fracture of left femur. (C) X–ray of skull showing ‘salt and pepper appearance’ of skull.
The classic bone disease of PHPT, OFC is seen in <2% of patients. In severe and long-standing disease, elevated PTH causes increased osteoclast activity resulting in localised alterations in the trabecular pattern, demineralisation and replacement of marrow by loose connective tissue, leading to radiographic disappearance of bones, as was seen in our patient. They are most commonly seen in flat bones, however, metacarpals and metatarsals are very rarely involved. Differentials of vanishing bone disease besides PHPT include osteomyelitis, Charcot's neuroarthropathy, rheumatoid arthritis, osseous metastasis and Gorham's disease.
Footnotes
Contributors VSS: managed the case and prepared the manuscript. AB: conceived the idea and edited the manuscript.
Competing interests None declared.
Patient consent Obtained.
- Provenance and peer review Not commissioned; externally peer reviewed.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd