- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Vaginal birth after cesarean associated with higher risks
Attempted vaginal birth after cesarean (VBAC) is associated with higher rates of maternal and infant morbidity and mortality as compared to elective repeat cesarean delivery, although absolute rates of such adverse outcomes are lower with VBAC, according to research in Canadian Medical Association Journal (CMAJ).
The research was conducted by Dr. Carmen Young and colleagues to compare maternal and infant outcomes after attempted vaginal birth after cesarean delivery versus elective repeat cesarean delivery.
VBAC is increasingly contentious as rates of cesarean delivery rise and prior cesarean delivery serves as the most common single indication for a cesarean delivery.
Elective repeat cesarean delivery is associated with an increased risk of:
- Surgical complications
- Abnormal placentation in subsequent pregnancies
Attempted vaginal birth after cesarean delivery is associated with:
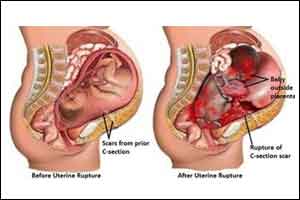
- Higher risk of uterine rupture
- Maternal and infant complications
So, planning mode of delivery for women with a previous cesarean delivery is challenging both for the patient and the care provider.
"The absolute rates of adverse maternal and neonatal outcomes are low with both attempted VBAC and elective repeat cesarean delivery," says Dr. Carmen Young, University of Alberta. "Both are reasonable options for women in general; however, attempted VBAC continues to be associated with higher relative rates of severe adverse maternal and neonatal outcomes compared with an elective repeat cesarean delivery."
Researchers conducted a study using information on all women in Canada (excluding Quebec) who had a previous cesarean delivery and subsequently delivered between 2003 and 2015. Logistic regression was used to estimate adjusted rate ratios (RRs) and 95% confidence intervals (CIs).
The investigators found that:
- Absolute rates of severe maternal morbidity and mortality were low but significantly higher after attempted VBAC compared with elective repeat cesarean delivery.
- Adjusted rate differences in severe maternal morbidity and mortality, and serious neonatal morbidity and mortality were small.
- The association between VBAC and serious neonatal morbidity and mortality showed a temporal worsening.
"For women who may be candidates for an attempted VBAC, the choice between an elective repeat cesarean delivery and an attempted VBAC depends on the woman's desire for a vaginal delivery, her tolerance for risk and whether she is planning a small or large family," says Dr. Young.
Based on the study the authors concluded that attempted vaginal birth after cesarean delivery is associated with low absolute rates of severe maternal and infant morbidity and mortality, although relative rates of such adverse outcomes are higher than for elective repeat cesarean delivery.
Temporal trends in the effects of attempted VBAC on serious neonatal morbidity and mortality have shown a concerning increase in recent years, and further study is required to identify the cause of this unexpected development. This study emphasizes the need to focus on an appropriate selection of candidates and careful monitoring of labor and delivery among women with a previous cesarean delivery that will ensure the safety of attempted vaginal birth after cesarean delivery.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd