- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Updated guideline on ulcerative colitis: American College of Gastroenterology
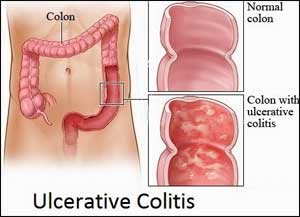
The American College of Gastroenterology has released an updated version of its clinical guideline on ulcerative colitis in adults. The guideline, last updated in 2010, is intended to present a framework for physicians to care for all patients with the condition throughout their disease course and includes takeaways that can be applied to practice quickly.
The guideline is published in The American Journal of Gastroenterology.
An emerging goal in ulcerative colitis management is mucosal healing, the guideline stated. Mucosal healing was defined as resolution of inflammatory changes (Mayo endoscopic subscore 0 or 1) and is key to increasing the likelihood of sustained steroid-free remission and preventing hospitalizations and surgery, the guideline said (conditional recommendation, low-quality evidence).
Key Recommendations:
- Management of ulcerative colitis must involve a prompt and accurate diagnosis, assessment of the patient's risk of poor outcomes, and initiation of effective, safe, and tolerable medical therapies.
- The optimal goal of management is a sustained and durable period of steroid-free remission, accompanied by appropriate psychosocial support, normal health-related quality of life (QoL), prevention of morbidity including hospitalization and surgery, and prevention of cancer.
- For diagnosis and assessment, the guideline recommends in favor of stool testing to rule out Clostridioides difficile (formerly Clostridium difficile) in patients with suspected ulcerative colitis but against serologic antibody testing to establish or rule out a diagnosis or determine the prognosis.
- Once remission is achieved, for patients with mildly active ulcerative proctitis, rectal 5-aminosalicylate (5-ASA) therapies at a dose of 1 g/d are recommended for induction of remission.
- For moderately to severely active ulcerative colitis, the guideline recommends oral budesonide multi-matrix (MMX) for induction of remission.
- The guideline recommended against both concomitant 5-ASA and systemic corticosteroids for maintenance of remission in patients with previously moderately to severely active disease who have achieved remission but in whom 5-ASA therapy previously failed and who are now on anti-tumor necrosis factor (TNF) therapy.
- For patients with previously moderately to severely active disease in remission from corticosteroids, thiopurines are recommended for maintenance of remission compared with no treatment or corticosteroids.
- The guideline also recommended against using methotrexate for maintenance of remission. Instead, it recommended continuing anti-TNF therapy using adalimumab, golimumab, or infliximab to maintain remission after anti-TNF induction in patients with previously moderately to severely active disease.
- The guideline also stressed follow-up for colorectal cancer screening and recommended that screening and subsequent surveillance colonoscopy begin eight years after diagnosis to assess for dysplasia in individuals with ulcerative colitis that involves more than the rectum.
- Patients with UC and primary sclerosing cholangitis should undergo a screening colonoscopy when diagnosed and surveillance annually.
- Surveillance colonoscopies should be performed at one- to three-year intervals based on the combined risk factors for colorectal cancer and findings from previous colonoscopies.
“Patients with [ulcerative colitis] are at an increased risk of [colorectal cancer] and should undergo surveillance colonoscopy focused on identifying and removing precancerous dysplasia,” the guideline said. “The evolution of technology has resulted in more directly visualized approaches, removal of endoscopically discrete lesions, and in select patients, active surveillance rather than proctocolectomy.
For further reference log on to 10.14309/ajg.0000000000000152

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd