- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Ulcerative colitis management: NICE 2019 Guidelines
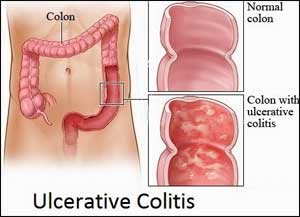
NICE has released 2019 guidelines on Ulcerative colitis management. This guideline covers the management of ulcerative colitis in children, young people and adults. It aims to help professionals to provide consistently high-quality care and it highlights the importance of advice and support for people with ulcerative colitis.
Following are the major recommendations:
Treating mild-to-moderate ulcerative colitis
Proctitis
- To induce remission in people with a mild-to-moderate first presentation or inflammatory exacerbation of proctitis, offer a topical aminosalicylate as first-line treatment. [2019]
- If remission is not achieved within 4 weeks, consider adding an oral aminosalicylate. [2019]
- If further treatment is needed, consider adding a time-limited course of a topical or an oral corticosteroid. [2019]
- For people who decline a topical aminosalicylate:
- consider an oral aminosalicylate as first-line treatment, and explain that this is not as effective as a topical aminosalicylate
- if remission is not achieved within 4 weeks, consider adding a time-limited course of a topical or an oral corticosteroid. [2019]
- For people who cannot tolerate aminosalicylates, consider a time-limited course of a topical or an oral corticosteroid. [2019]
Proctosigmoiditis and left-sided ulcerative colitis
- To induce remission in people with a mild-to-moderate first presentation or inflammatory exacerbation of proctosigmoiditis or left-sided ulcerative colitis, offer a topical aminosalicylate as first-line treatment. [2019]
- If remission is not achieved within 4 weeks, consider:
- adding a high-dose oral aminosalicylate to the topical aminosalicylate or
- switching to a high-dose oral aminosalicylate and a time-limited course of a topical corticosteroid. [2019]
- If further treatment is needed, stop topical treatments and offer an oral aminosalicylate and a time-limited course of an oral corticosteroid. [2019]
- For people who decline any topical treatment:
- consider a high-dose oral aminosalicylate alone, and explain that this is not as effective as a topical aminosalicylate
- if remission is not achieved within 4 weeks, offer a time-limited course of an oral corticosteroid in addition to the high-dose aminosalicylate. [2019]
- For people who cannot tolerate aminosalicylates, consider a time-limited course of a topical or an oral corticosteroid. [2019]
Extensive disease
- To induce remission in people with a mild-to-moderate first presentation or inflammatory exacerbation of extensive ulcerative colitis, offer a topical aminosalicylate and a high-dose oral aminosalicylate as first-line treatment. [2019]
- If remission is not achieved within 4 weeks, stop the topical aminosalicylate and offer a high-dose oral aminosalicylate with a time-limited course of an oral corticosteroid. [2019]
- For people who cannot tolerate aminosalicylates, consider a time-limited course of an oral corticosteroid. [2019]
Biologics and Janus kinase inhibitors for moderately to severely active ulcerative colitis: all extents of disease
- For guidance on biologics and Janus kinase inhibitors for treating moderately to severely active ulcerative colitis, see the NICE technology appraisal guidance on:
- infliximab, adalimumab and golimumab for moderately to severely active ulcerative colitis
- vedolizumab for treating moderately to severely active ulcerative colitis
- tofacitinib for moderately to severely active ulcerative colitis. [2019]
Treating acute severe ulcerative colitis: all extents of disease
The multidisciplinary team
- For people admitted to hospital with acute severe ulcerative colitis:
- ensure that a gastroenterologist and a colorectal surgeon collaborate to provide treatment and management
- ensure that the composition of the multidisciplinary team is appropriate for the age of the person
- seek advice from a paediatrician with expertise in gastroenterology when treating a child or young person
- ensure that the obstetric and gynaecology team is included when treating a pregnant woman. [2013]
Step 1 therapy
- For people admitted to hospital with acute severe ulcerative colitis (either a first presentation or an inflammatory exacerbation):
- offer intravenous corticosteroids to induce remission and
- assess the likelihood that the person will need surgery. [2013]
- Consider intravenous ciclosporin or surgery for people:
- who cannot tolerate or who decline intravenous corticosteroids or
- for whom treatment with intravenous corticosteroids is contraindicated.
Take into account the person's preferences when choosing treatment. [2013]
Step 2 therapy
- Consider adding intravenous ciclosporin to intravenous corticosteroids or consider surgery for people:
- who have little or no improvement within 72 hours of starting intravenous corticosteroids or
- whose symptoms worsen at any time despite corticosteroid treatment.
Take into account the person's preferences when choosing treatment. [2013]
- Infliximab is recommended as an option for the treatment of acute exacerbations of severely active ulcerative colitis only in patients in whom ciclosporin is contraindicated or clinically inappropriate, based on a careful assessment of the risks and benefits of treatment in the individual patient. [2008]
- In people who do not meet the criterion in 1.2.19, infliximab should only be used for the treatment of acute exacerbations of severely active ulcerative colitis in clinical trials. [2008]
Monitoring treatment
- Ensure that there are documented local safety monitoring policies and procedures (including audit) for adults, children and young people receiving treatment that needs monitoring (aminosalicylates, tacrolimus, ciclosporin, infliximab, azathioprine and mercaptopurine). Nominate a member of staff to act on abnormal results and communicate with GPs and people with ulcerative colitis and their family members or carers (as appropriate). [2013]
Assessing likelihood of needing surgery
- Assess and document on admission, and then daily, the likelihood of needing surgery for people admitted to hospital with acute severe ulcerative colitis. [2013]
- Be aware that there may be an increased likelihood of needing surgery for people with any of the following:
- stool frequency more than 8 per day
- pyrexia
- tachycardia
- an abdominal X‑ray showing colonic dilatation
- low albumin, low haemoglobin, high platelet count or C‑reactive protein above 45 mg/litre (bear in mind that normal values may be different in pregnant women). [2013]
3. Information about treatment options for people who are considering surgery
These recommendations apply to anyone with ulcerative colitis considering elective surgery. The principles can also be applied to people requiring emergency surgery.
Information when considering surgery
- For people with ulcerative colitis who are considering surgery, ensure that a specialist (such as a gastroenterologist or a nurse specialist) gives the person and their family members or carers (as appropriate) information about all available treatment options, and discusses this with them. Information should include the benefits and risks of the different treatments and the potential consequences of no treatment. [2013]
- Ensure that the person and their family members or carers (as appropriate) have sufficient time and opportunities to think about the options and the implications of the different treatments. [2013]
- Ensure that a colorectal surgeon gives any person who is considering surgery and their family members or carers (as appropriate) specific information about what they can expect in the short and long term after surgery, and discusses this with them. [2013]
- Ensure that a specialist (such as a colorectal surgeon, a gastroenterologist, an inflammatory bowel disease nurse specialist or a stoma nurse) gives any person who is considering surgery and their family members or carers (as appropriate) information about:
- diet
- sensitive topics such as sexual function
- effects on lifestyle
- psychological wellbeing
- the type of surgery, the possibility of needing a stoma and stoma care. [2013]
- Ensure that a specialist who is knowledgeable about stomas (such as a stoma nurse or a colorectal surgeon) gives any person who is having surgery and their family members or carers (as appropriate) specific information about the siting, care and management of stomas. [2013]
Information after surgery
- After surgery, ensure that a specialist who is knowledgeable about stomas (such as a stoma nurse or a colorectal surgeon) gives the person and their family members or carers (as appropriate) information about managing the effects on bowel function. This should be specific to the type of surgery performed (ileostomy or ileoanal pouch) and could include the following:
- strategies to deal with the impact on their physical, psychological and social wellbeing
- where to go for help if symptoms occur
- sources of support and advice. [2013]
4. Maintaining remission in people with ulcerative colitis
Proctitis and proctosigmoiditis
- To maintain remission after a mild-to-moderate inflammatory exacerbation of proctitis or proctosigmoiditis, consider the following options, taking into account the person's preferences:
- a topical aminosalicylate alone (daily or intermittent) or
- an oral aminosalicylate plus a topical aminosalicylate[1] (daily or intermittent) or
- an oral aminosalicylate alone, explaining that this may not be as effective as combined treatment or an intermittent topical aminosalicylate alone. [2013]
Left-sided and extensive ulcerative colitis
- To maintain remission in adults after a mild-to-moderate inflammatory exacerbation of left-sided or extensive ulcerative colitis:
- offer a low maintenance dose of an oral aminosalicylate
- when deciding which oral aminosalicylate to use, take into account the person's preferences, side effects and cost. [2013]
- To maintain remission in children and young people after a mild-to-moderate inflammatory exacerbation of left-sided or extensive ulcerative colitis:
- offer an oral aminosalicylate
- when deciding which oral aminosalicylate to use, take into account the person's preferences (and those of their parents or carers as appropriate), side effects and cost. [2013]
All extents of disease
- Consider oral azathioprine or oral mercaptopurine to maintain remission:
- after 2 or more inflammatory exacerbations in 12 months that require treatment with systemic corticosteroids or
- if remission is not maintained by aminosalicylates. [2013]
- To maintain remission after a single episode of acute severe ulcerative colitis:
- consider oral azathioprine or oral mercaptopurine
- consider oral aminosalicylates if azathioprine and/or mercaptopurine are contraindicated or the person cannot tolerate them. [2013]
Dosing regimen for oral aminosalicylates
- Consider a once-daily dosing regimen for oral aminosalicylates[7] when used for maintaining remission. Take into account the person's preferences, and explain that once-daily dosing can be more effective, but may result in more side effects. [2013]
5. Pregnant women
- When caring for a pregnant woman with ulcerative colitis:
- Ensure effective communication and information-sharing across specialties (for example, primary care, obstetrics and gynaecology, and gastroenterology).
- Give her information about the potential risks and benefits of medical treatment to induce or maintain remission and of not having treatment, and discuss this with her. Include information relevant to a potential admission for an acute severe inflammatory exacerbation. [2013]
6. Monitoring
Monitoring bone health
Adults
- For recommendations on assessing the risk of fragility fracture in adults, refer to the NICE guideline on osteoporosis: assessing the risk of fragility fracture. [2013]
Children and young people
- Consider monitoring bone health in children and young people with ulcerative colitis in the following circumstances:
- during chronic active disease
- after treatment with systemic corticosteroids
- after recurrent active disease. [2013]
Monitoring growth and pubertal development in children and young people
- Monitor the height and body weight of children and young people with ulcerative colitis against expected values on centile charts (and/or z scores) at the following intervals according to disease activity:
- every 3 to 6 months:
- if they have an inflammatory exacerbation and are approaching or undergoing puberty or
- if there is chronic active disease or
- if they are being treated with systemic corticosteroids
- every 6 months during pubertal growth if the disease is inactive
- every 12 months if none of the criteria above are met. [2013]
- Monitor pubertal development in young people with ulcerative colitis using the principles of Tanner staging, by asking screening questions and/or carrying out a formal examination. [2013]
- Consider referral to a secondary care paediatrician for pubertal assessment and investigation of the underlying cause if a young person with ulcerative colitis:
- has slow pubertal progress or
- has not developed pubertal features appropriate for their age. [2013]
- Monitoring of growth and pubertal development:
- can be done in a range of locations (for example, at routine appointments, acute admissions or urgent appointments in primary care, community services or secondary care)
- should be carried out by appropriately trained healthcare professionals as part of the overall clinical assessment (including disease activity) to help inform the need for timely investigation, referral and/or interventions, particularly during pubertal growth.
If the young person prefers self-assessment for monitoring pubertal development, this should be allowed if possible and they should be instructed on how to do this. [2013]
- Ensure that relevant information about monitoring of growth and pubertal development and about disease activity is shared across services (for example, community, primary, secondary and specialist services). Apply the principles in the NICE guideline on patient experience in adult NHS services in relation to continuity of care. [2013]
For more details click on the link: www.nice.org.uk

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd