- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Tuberculosis of Spine- Standard Treatment Guidelines
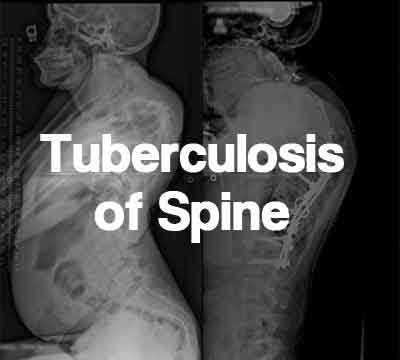
India is classified as a country with a high burden and the least prospects of a favourable time trend of the disease. The average prevalence of all forms of tuberculosis in India is estimated to be 5 per thousand. Skeletal tuberculosis is found in 1 to 3 % of these cases. Spine might be involved in upto 50% of these cases. Neurological complications and progressive deformity are the dreaded complications of tuberculosis of spine. It is imperative to diagonose this condition early and initiate early medical treatment while recognising and treating patients requiring surgical interventions for optimal outcomes.
The Ministry of Health and Family Welfare has issued the standard treatment Orthopaedics Guidelines for Tuberculosis of Spine. Following are the major recommendations:
The average prevalence of all forms of tuberculosis in India is estimated to be 5 per thousand Skeletal system involvement occurs in 1% to 3% of the patients and up to 50% of these affected patients have TB of the spine
Tumours of spine
Prevention would entail measures as for other forms of tuberculosis. Osteoarticular tuberculosis is always secondary, so primary infection should be treated effectively for sufficient time. Once diagnosed, close follow up, regular anti tubercular treatment and aggressive surgical approach may prevent dreaded complications
Clinical Diagnosis:
The presentation depends on the following:
Stage of disease
Affected site
Presence of complications
Back pain is the earliest and most common symptom. Any back pain not responding to conservative treatment for more than 6 weeks and/or accompanied by constitutional symptoms should be investigated further Neurologic abnormalities occur in 50% of cases and can include paraplegia, paresis, impaired sensation, nerve root pain. Patients with cervical spine disease can present with dysphagia or stridor.Symptoms can also include torticollis, hoarseness, and neurologic deficits.
The examination should include the following:
Assessment of spinal deformity Inspection of skin, with attention to detection of sinuses and subcutaneous mass indicating cold abscess Meticulous neurologic examination
Investigations:
The erythrocyte sedimentation rate (ESR) is elevated. IgM for mycobacterium tuberculosis can be done.HIV status should be confirmed. Microbiology studies can be used to confirm diagnosis. Aspirates of cold abscees can be obtained to stain for acid-fast bacilli (AFB).
The following are radiographic changes characteristic of spinal tuberculosis
Treatment:
Goals of management in active tuberculosis
Eradication/ Control of Disease
Decompression of spinal cord
Prevention of progressive deformity and later neurological
complications Early mobilization of the patient.
Treatment options
Chemotherapy alone (long course is preferred)
Surgery with Chemotherapy
Standard Operating procedure
In Patient
In patients without deficit,chemotherapy alone is sufficient if the risk of progressive deformity is not there. Inpatient care might be needed initially for patients who are undergoing treatment to ensure rest and monitor response to ATT. A close watch on development of neurological symptoms is to be kept and at signs of deterioration, the patient may be referred.
Out Patient
Patients on ATT are to be followed closely for progression of deformity and deterioration of neurological deficit
Day Care
Patients needing drainage of cold abscess may be kept in day care.
Referral criteria:
Clinical Diagnosis:
The presentation depends on the following:
Stage of disease
Affected site
Presence of complications
Back pain is the earliest and most common symptom. Any back pain not responding to conservative treatment for more than 6 weeks and/or accompanied by constitutional symptoms should be investigated further Neurologic abnormalities occur in 50% of cases and can include paraplegia, paresis, impaired sensation, nerve root pain. Patients with cervical spine disease can present with dysphagia or stridor.Symptoms can also include torticollis, hoarseness, and neurologic deficits.
The examination should include the following:
Assessment of spinal deformity Inspection of skin, with attention to detection of sinuses and subcutaneous mass indicating cold abscess Meticulous neurologic examination
Investigations:
Routine blood investigation,Tb-PCR, In MDR Tb-culture and sensitivity MRI is the most effective imaging study for demonstrating neural compression. MRI is standard for evaluating disk-space infection and osteomyelitis of the spine and is most effective for demonstrating the extension of disease into soft tissues and the spread of tuberculous debris under the anterior and posterior longitudinal ligaments. CT scanning provides much better bony detail of irregular lytic lesions, sclerosis, disk collapse, and disruption of bone circumference. CT guided biopsy maybe done in case of doubtful diagonoses.
Treatment:
Standard Operating procedure
In Patient
Tuberculosis spine with no neurological deficit Chemotherapy alone is sufficient if there is no risk of progressive deformity Efforts should be made to identify patients who are at risk of developing kyphosis in active disease. Growing children with dorsal and dorsolumbar caries with more than 3 body involvement or in which there is destruction more than 1.5 times the vertebral body height are at risk of kyphosis.
Indications of surgery
Failure to respond to conservative treatment
Deformity/risk of progresion
Recurrence of the disease
Doubtful diagonosis
Tuberculosis spine with neurological deficit Middle path regime In patients with mild deficit trial of chemotherapy can be done, however a close observation is must.
Indications for surgery for management of tuberculosis with deficit
Severe neurologic symptoms Progressive neurologic symptoms Unsuccessful nonoperative treatment Instability with spinal deformity, Spinal tumour syndrome.
Operative treatment of tuberculosis spine
Out Patient
Regular follow up of operated patients as well as patients on conservative treatment. At each follow-up detailed neurological examination should be performed and serial x rays should be taken and deformity progression should be noted.
Regular biochemical investigations for monitoring ATT
Day Care
For drainage of cold abscesses when needed
WHO DOES WHAT? and TIMELINES
Doctor
Nurse
Technician
Development Team Dr. P.K. DAVE, Rockland Hospital, New Delhi Dr. P.S. Maini, Fortis Jessa Ram Hospital, New Delhi
The Ministry of Health and Family Welfare has issued the standard treatment Orthopaedics Guidelines for Tuberculosis of Spine. Following are the major recommendations:
Incidence of the condition in Our Country
The average prevalence of all forms of tuberculosis in India is estimated to be 5 per thousand Skeletal system involvement occurs in 1% to 3% of the patients and up to 50% of these affected patients have TB of the spine
Differential Diagnosis
Tumours of spine
Traumatic conditions
Other infectious afflictions of spine like brucella, pyogenic.
Prevention and Counselling
Prevention would entail measures as for other forms of tuberculosis. Osteoarticular tuberculosis is always secondary, so primary infection should be treated effectively for sufficient time. Once diagnosed, close follow up, regular anti tubercular treatment and aggressive surgical approach may prevent dreaded complications
Optimal Diagnostic Criteria, Investigations, Treatment and Referral Criteria At Secondary Hospital
Clinical Diagnosis:
The presentation depends on the following:
Stage of disease
Affected site
Presence of complications
Back pain is the earliest and most common symptom. Any back pain not responding to conservative treatment for more than 6 weeks and/or accompanied by constitutional symptoms should be investigated further Neurologic abnormalities occur in 50% of cases and can include paraplegia, paresis, impaired sensation, nerve root pain. Patients with cervical spine disease can present with dysphagia or stridor.Symptoms can also include torticollis, hoarseness, and neurologic deficits.
The examination should include the following:
Assessment of spinal deformity Inspection of skin, with attention to detection of sinuses and subcutaneous mass indicating cold abscess Meticulous neurologic examination
Investigations:
The erythrocyte sedimentation rate (ESR) is elevated. IgM for mycobacterium tuberculosis can be done.HIV status should be confirmed. Microbiology studies can be used to confirm diagnosis. Aspirates of cold abscees can be obtained to stain for acid-fast bacilli (AFB).
The following are radiographic changes characteristic of spinal tuberculosis
- Paradiscal involvement with decreased disc space
- Increased anterior wedging
- Collapse of vertebral body
- Enlarged psoas shadow with or without calcification
- Fusiform paravertebral shadows suggest abscess formation
Treatment:
Goals of management in active tuberculosis
Eradication/ Control of Disease
Decompression of spinal cord
Prevention of progressive deformity and later neurological
complications Early mobilization of the patient.
Treatment options
Chemotherapy alone (long course is preferred)
Surgery with Chemotherapy
- Antero-Lateral Decompression
- Antero-Lateral Decompression + post fusion Antero-Lateral Decompression + strut grafting+post fusion
- Ant. Decompression + strut grafting+posterior instrumentation
- Ant. Decompression + strut grafting + instrumentation
Standard Operating procedure
In Patient
In patients without deficit,chemotherapy alone is sufficient if the risk of progressive deformity is not there. Inpatient care might be needed initially for patients who are undergoing treatment to ensure rest and monitor response to ATT. A close watch on development of neurological symptoms is to be kept and at signs of deterioration, the patient may be referred.
Out Patient
Patients on ATT are to be followed closely for progression of deformity and deterioration of neurological deficit
Day Care
Patients needing drainage of cold abscess may be kept in day care.
Referral criteria:
- Failure to respond to conservative treatment
- Deformity/risk of progresion
- Recurrence of the disease
- Doubtful diagonosis
- Severe neurologic symptoms
- Progressive neurologic symptoms inspite of ATT
- Unsuccessful nonoperative treatment
- Instability with spinal deformity,
- Spinal tumour syndrome.
At Super Specialty Hospital
Clinical Diagnosis:
The presentation depends on the following:
Stage of disease
Affected site
Presence of complications
Back pain is the earliest and most common symptom. Any back pain not responding to conservative treatment for more than 6 weeks and/or accompanied by constitutional symptoms should be investigated further Neurologic abnormalities occur in 50% of cases and can include paraplegia, paresis, impaired sensation, nerve root pain. Patients with cervical spine disease can present with dysphagia or stridor.Symptoms can also include torticollis, hoarseness, and neurologic deficits.
The examination should include the following:
Assessment of spinal deformity Inspection of skin, with attention to detection of sinuses and subcutaneous mass indicating cold abscess Meticulous neurologic examination
Investigations:
Routine blood investigation,Tb-PCR, In MDR Tb-culture and sensitivity MRI is the most effective imaging study for demonstrating neural compression. MRI is standard for evaluating disk-space infection and osteomyelitis of the spine and is most effective for demonstrating the extension of disease into soft tissues and the spread of tuberculous debris under the anterior and posterior longitudinal ligaments. CT scanning provides much better bony detail of irregular lytic lesions, sclerosis, disk collapse, and disruption of bone circumference. CT guided biopsy maybe done in case of doubtful diagonoses.
Treatment:
Standard Operating procedure
In Patient
Tuberculosis spine with no neurological deficit Chemotherapy alone is sufficient if there is no risk of progressive deformity Efforts should be made to identify patients who are at risk of developing kyphosis in active disease. Growing children with dorsal and dorsolumbar caries with more than 3 body involvement or in which there is destruction more than 1.5 times the vertebral body height are at risk of kyphosis.
Indications of surgery
Failure to respond to conservative treatment
Deformity/risk of progresion
Recurrence of the disease
Doubtful diagonosis
Tuberculosis spine with neurological deficit Middle path regime In patients with mild deficit trial of chemotherapy can be done, however a close observation is must.
Indications for surgery for management of tuberculosis with deficit
Severe neurologic symptoms Progressive neurologic symptoms Unsuccessful nonoperative treatment Instability with spinal deformity, Spinal tumour syndrome.
Operative treatment of tuberculosis spine
- Anterolateral decompression alone will lead to control of disease and adequate decompression but there might be progression of kyphotic deformity
- ALD should ideally be accompanied by posterior fusion and anterior structural graft.By providing structural support and by its osteogenic potential, the graft may prevent progression of kyphosis.
- Anterior debridement and arthrodesis by graft only may result in permanent kyphotic deformity as a consequence of fracture of the graft, slippage of the graft out of its bed, resorption of the graft,or subsidence of the graft into the cancellous vertebral bodies. Anterior grafting procedure should be accompanied by instrumentation either anterior or posterior.
- Instrumentation has been shown to be safe in tuberculosis and it helps in stability of graft, early fusion and rapid mobilisation of the patient.
- Anterior structural graft that can be used are tricortical iliac crest, fibula, ribs or bone impregnated titanium mesh.
- Direct anterior approach (transthoracic, retroperitoneal) is a formidable procedure and intensive care facilities should be available.
- In a healed disease, severe kyphosis correction is fraught with danger as spinal cord has exhausted its reserve
Out Patient
Regular follow up of operated patients as well as patients on conservative treatment. At each follow-up detailed neurological examination should be performed and serial x rays should be taken and deformity progression should be noted.
Regular biochemical investigations for monitoring ATT
Day Care
For drainage of cold abscesses when needed
WHO DOES WHAT? and TIMELINES
Doctor
- Clinical diagnoses
- Investigations
- Clinical decision making
- Surgical procedure
- Maintenance of record and follow up
Nurse
- Councelliung
- Surgical assistance
Technician
- Investigations
- Helps in surgery
- Orthosis
RESOURCES REQUIRED FOR ONE PATIENT
| Situation | Human Resources | Investigation | Drugs and Consumables | Equipmemnts |
| Orthopedic surgeon | X rays Microbiology and biochemistry labs | ATT Braces | ||
| Team of surgeons with training in spinal surgery Nurses for OT assistance, ward work and OPD follow up | X rays CT MRI Microbiology with provision for advances culture techniques Biochemistry | ATT OT inventory Spinal instrumentation | Well equipped OTS with ICU backup. |
Development Team Dr. P.K. DAVE, Rockland Hospital, New Delhi Dr. P.S. Maini, Fortis Jessa Ram Hospital, New Delhi
GOI guidelinesguidelinesMinistry of Health and Family WelfareOrthopaedics GuidelinesSpinal TBspine TuberculosisStandard Treatment GuidelinesTBTB spinetreatment guidelinesTuberculosis
Next Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd