- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Trends and outcomes of off-label use of TAVR
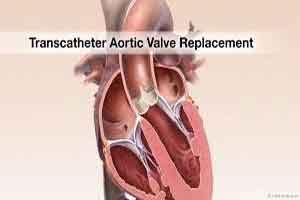
Transcatheter aortic valve replacement (TAVR) was approved by the US Food and Drug Administration (FDA) for severe aortic stenosis in patients who cannot undergo surgery and for patients at high operative risk. TAVR is not currently recommended owing to limited proof of efficacy in patients with low surgical risk for surgical aortic valve replacement (AVR), known bicuspid aortic valve, severe mitral regurgitation, moderate aortic stenosis, severe aortic regurgitation, or subaortic stenosis. The use and outcomes of TAVR of off-label indications has not been previously reported.
Hira et al used data from the NCDR STS/ACC Transcatheter Valve Therapy (TVT) Registry launched in November 2011 to evaluate patterns and outcomes of off-label TAVR use in the US.
From a total of 23,847 patients who underwent TAVR between November 2011 and September 2014 at 328 sites, off-label use was identified in 2,272 patients (9.5%). Off-label TAVR was defined as TAVR in patients with known bicuspid valve, moderate aortic stenosis, severe mitral regurgitation, severe aortic regurgitation, or subaortic stenosis.
Unadjusted in-hospital mortality was higher 6.3% among patients receiving off-label TAVR compared to 4.7% for those receiving on-label TAVR (p<0.001). Thirty-day mortality was 8.5% vs. 6.1%, respectively (p<0.001); 30-day heart failure was 5.8% vs. 4.3%, respectively (p=0.01), and one-year mortality was 25.6% vs. 22.1%, respectively (p=0.001).
After multivariate adjustment, 30-day mortality was still higher in the off-label group (hazard ratio, 1.27; p=0.02), but 1-year mortality was similar (HR, 1.11; p=0.11). In-hospital, 30-day, and 1-year mortality was highest in patients with severe mitral regurgitation as the only off-label indication.
The median rate of off-label TAVR use per hospital was 6.8% (range, 0% to 34.7%). Hospitals in the highest tertile of off-label use had longer mean duration of participation in the TVT registry and also had increased absolute 30-day event rates compared to those in the lowest tertile of off-label use. However, after adjustment, 30-day and 1-year composite adverse events were no lower significantly higher in centers that did more off-label TAVR.
The investigators found that between November 2011 and September 2014, about 1 in 10 patients with the US have received TAVR for an off-label indication, albeit with wide variation in this practice seen among different hospitals. While unadjusted 30-day and 1-year mortality were both higher in those who received off-label TAVR, the difference at one-year was no longer significant after multivariate adjustment. Additional research on the safety and efficacy of off-label TAVR is needed.
Reference
1. R S Hira, S Vemulapalli, Z Li, et al: Trends and Outcomes of Off-Label Use of Transcatheter Aortic Valve Replacement: Insights From the NCDR STS/ACC TVT Registry. JAMA Cardiol. Jun 21, 2017. (Published online ahead of print.) 28636718

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd