- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
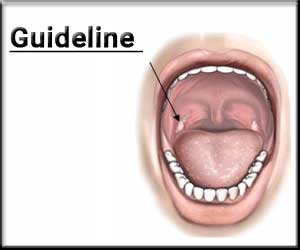
Tonsillectomy in children: Updated AAO-HNSF Guideline
The American Academy of Otolaryngology–Head and Neck Surgery Foundation (AAO-HNSF) has released an updated version of its guideline on tonsillectomy in children. The guideline, published in the journal Otolaryngology-Head and Neck Surgery is intended for all clinicians in any setting who interact with children who may be candidates for tonsillectomy.
Tonsillectomy is defined as a surgical procedure performed with or without adenoidectomy that completely removes the tonsil, including its capsule, by dissecting the peritonsillar space between the tonsil capsule and the muscular wall. The procedure is commonly performed for recurrent throat infections and obstructive sleep apnea.
The purpose of this multidisciplinary guideline is to identify quality improvement opportunities in managing children under consideration for tonsillectomy and to create explicit and actionable recommendations to implement these opportunities in clinical practice.
Recurrent Throat Infection
- Clinicians should recommend watchful waiting for recurrent throat infection if there have been fewer than seven episodes in the past year, fewer than five episodes per year in the past 2 years, or fewer than three episodes per year in the past 3 years.
- Clinicians may recommend tonsillectomy for recurrent throat infection with a frequency of at least seven episodes in the past year, at least five episodes per year for 2 years, or at least three episodes per year for 3 years with documentation in the medical record for each episode of sore throat and at least one of the following: temperature higher than 38.3°C (101°F), cervical adenopathy, tonsillar exudate, or positive test for group A beta-hemolytic streptococcus.
- In a child with recurrent throat infection who does not meet the criteria in the preceding statement, clinicians should assess for modifying factors that may nonetheless favour tonsillectomy. Such factors may include but are not limited to, multiple antibiotic allergies/intolerance, PFAPA (periodic fever, aphthous stomatitis, pharyngitis, and adenitis), or a history of more than one peritonsillar abscess.
Obstructive Sleep-Disordered Breathing and Obstructive Sleep Apnea
- Clinicians should ask caregivers of children with obstructive sleep-disordered breathing (oSDB) and tonsillar hypertrophy about comorbid conditions that may improve after tonsillectomy, including growth retardation, poor school performance, enuresis, asthma, and behavioural problems.
- Before performing tonsillectomy, the clinician should refer children with oSDB for polysomnography (PSG) if they are younger than 2 years or if they exhibit any of the following: obesity, Down syndrome, craniofacial abnormalities, neuromuscular disorders, sickle cell disease, or mucopolysaccharidoses.
- The clinician should advocate for PSG prior to tonsillectomy for oSDB in children without any of the comorbidities listed in the preceding statement when the need for tonsillectomy is uncertain or when there is discordance between the physical examination and the reported severity of oSDB.
- Clinicians should recommend tonsillectomy for children with obstructive sleep apnea (OSA) documented by overnight PSG.
- Clinicians should counsel patients and caregivers and explain that oSDB may persist or recur after tonsillectomy and may require further management.
Perioperative Care
- The clinician should counsel patients and caregivers regarding the importance of managing posttonsillectomy pain as part of the perioperative education process and should reinforce this counselling at the time of surgery with reminders about the need to anticipate, reassess, and adequately treat pain after surgery.
- Clinicians should not administer or prescribe perioperative antibiotics to children undergoing tonsillectomy.
- Clinicians should administer a single intraoperative dose of intravenous dexamethasone to children undergoing tonsillectomy.
- Clinicians should arrange for overnight inpatient monitoring of children after tonsillectomy if they are younger than 3 years or have severe OSA (apnea-hypopnea index [AHI] ≥10 obstructive events/hr, oxygen saturation nadir < 80%, or both).
- Clinicians should recommend ibuprofen, acetaminophen, or both for pain control after tonsillectomy.
- Clinicians must not administer or prescribe codeine or any medication containing codeine after tonsillectomy in children younger than 12 years.
Posttonsillectomy Bleeding
- Clinicians should follow up with patients and/or caregivers after tonsillectomy and document in the medical record the presence or absence of bleeding within 24 hours of surgery (primary bleeding) and bleeding occurring later than 24 hours after surgery (secondary bleeding).
- Clinicians should determine their rates of primary and secondary posttonsillectomy bleeding at least annually.
For full access to the guideline follow the link: https://doi.org/10.1177/0194599818801757

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd