- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Timing of melanoma diagnosis, treatment critical to survival
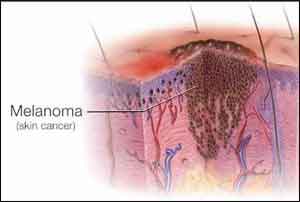
A new Cleveland Clinic study underscores the importance of early detection and treatment of melanoma, the deadliest form of skin cancer. The research, published online today in the Journal of the American Academy of Dermatology, indicates that the sooner patients were treated, the better their survival, particularly for stage I melanoma.
Using the National Cancer Database, researchers from Cleveland Clinic's Dermatology & Plastic Surgery Institute studied 153,218 adult patients diagnosed with stage I-III melanoma from 2004 to 2012 and found that overall survival decreased in patients waiting longer than 90 days for surgical treatment, regardless of stage. In addition, the delay of surgery beyond the first 29 days negatively impacted overall survival for stage I melanoma, though not for stage II or III.
Compared to patients who were treated within 30 days, patients with stage I melanoma were 5 percent more likely to die when treated between 30 and 59 days; 16 percent more likely to die when treated between 60 and 89 days; 29 percent more likely to die when treated between 91 and 120 days; and 41 percent more likely to die when treated after 120 days. Patients with a longer time to treatment initiation tended to be older and male, and have more comorbidities.
According to the authors, it is likely that more advanced cases represent delays in diagnosis, and these delays overwhelm the impact of a speedier treatment. However, in early stage cases, early diagnosis allows for the opportunity to improve the chances of survival with a prompt surgery. Although many physicians follow a rule-of-thumb to treat melanoma surgically three to four weeks after diagnosis, there is no official recommendation on time to treatment.
"The ideal timing for melanoma treatment, predominantly surgery, had yet to be determined - until now," said Brian Gastman, M.D., a plastic surgeon, director of melanoma surgery at Cleveland Clinic, and the primary investigator on the study. "Patients and referring physicians are not only concerned with how a melanoma is removed, but also when it's removed. We saw significantly worse prognoses and outcomes for those surgically treated after 30 days of stage I melanoma diagnosis. Knowing for certain that a more expedient time to surgery to remove an early melanoma improves the chances of survival is a game-changer in treating this life-threatening skin cancer."
Melanoma rates are on the rise, and it's estimated that 161,790 new cases of the disease will be diagnosed in the U.S. this year. On average, one American dies of melanoma every hour.
The study is a stark reminder of the importance of detecting skin cancer early, when it's most treatable. The American Academy of Dermatology encourages everyone to regularly examine their skin for signs of skin cancer, including the ABCDEs of melanoma:
- ASYMMETRY: Is one half of a mole unlike the other half?
- BORDER: Does a mole have an irregular, scalloped or poorly defined border?
- COLOR: It there more than one color in a mole, such as shades of tan and brown, black, white, red or blue?
- DIAMETER: Is a mole bigger than 6 mm (the size of a pencil eraser)? Melanomas are usually bigger than 6 mm when diagnosed, but they can be smaller.
- EVOLVING: Does a mole or another spot on the skin that look different from the rest? Is a mole or another spot is changing in size, shape or color?
Anyone who notices any new, changing or suspicious spots on their skin, or any spots that are changing, itching or bleeding, should see a board-certified dermatologist for diagnosis.
Because many physicians may be involved in the treatment of stage I melanoma -including general practitioners, dermatologists, general surgeons, surgical oncologists and plastic surgeons, among others - it's important for the entire medical community to be aware of the danger of melanoma and provide prompt treatment. In addition, patients should be prepared to be their own health advocates to prevent delays in their treatment.
The public can also take steps to reduce their melanoma risk by protecting themselves from exposure to harmful ultraviolet radiation from the sun and indoor tanning beds, a risk factor for all types of skin cancer. The AAD recommends that everyone protect their skin from the sun by seeking shade, wearing protective clothing and using a broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd