- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Thoracic aortic aneurysms exerting extreme pressure on the airway- A case study

Dr Hanna Jung at Department of Thoracic and Cardiovascular Surgery, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Republic of Korea have reported a rare case of thoracic aortic aneurysms exerting extreme pressure on the airway. The case has appeared in the Journal of Cardiothoracic Surgery.
An aneurysm is a localized or diffuse dilation of an artery with a diameter of at least 50% greater than the normal size of the artery. Thoracic aortic aneurysms, although mostly asymptomatic, are life-threatening owing to the risk of rupture. Moreover, the extrinsic pressure of a ruptured aneurysm may encroach the mediastinum. Dissection of a thoracic aortic aneurysm can lead to aneurysmal change and early or late rupture which may cause compression on airways as what happened in the instant case.
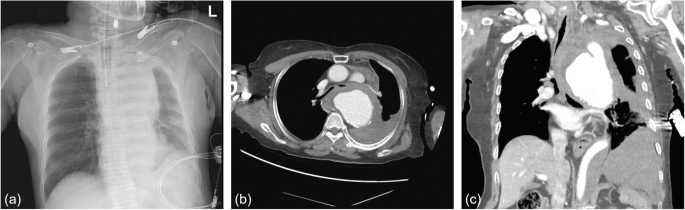
A 74-year-old woman with sudden chest pain and dyspnea was admitted to the emergency room and intubated on arrival owing to disturbed consciousness. She had hypertension but no history of asthma or chronic obstructive pulmonary disease. Chest radiography showed mediastinal widening (Fig. 1a). Computed tomography (CT) of the chest revealed rupture of the descending thoracic aortic aneurysm, which compressed the lower trachea and both main bronchi. The maximal diameter of the aneurysm at the level of the carina was 9 cm (Fig. 1b, c).
Even with aneurysmal rupture, after intubation and during the diagnosis, her vital signs were maintained stable enough to be transferred to our hospital. We performed an emergency thoracic endovascular aortic repair (TEVAR, seal stent-graft S&G Biotech Inc., Yongin-si, Korea, proximal 34 × 30 × 110 and distal 28 × 110). TEVAR was performed uneventfully and following admission to the intensive care unit, her vital signs were stable.
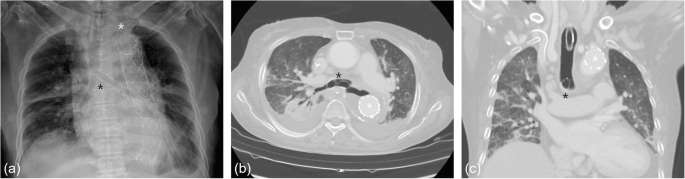
However, even with the mechanical ventilator support, carbon dioxide (CO2) retention was not easily resolved, and sudden oxygen desaturation with unusually high airway pressure and low tidal volume was repeated. Moreover, the suction tube was difficult or unable to pass the endotracheal tube. We were aware that the patient had airway compression in the initial CT, but anticipated that the extrinsic compression pressure of the ruptured aneurysm would be relieved after the TEVAR. Due to the failure to wean the patient from the mechanical ventilator, the follow-up chest CT was performed. Despite the stent-graft in the aorta (Fig. 2a), the hematoma of the ruptured aneurysm continued compressing the lower trachea and both main bronchi (Fig. 2b, c).

We planned to insert a silicone bronchial stent under rigid bronchoscopy. However, after the removal of the endotracheal tube, the rigid bronchoscopy was unable to enter the trachea. Further, re-intubation was not possible even with the anesthesiologist owing to the extrinsic pressure on the airway. Because the patient crashed owing to respiratory failure, she immediately underwent veno-veno extracorporeal membrane oxygenation (VV ECMO) support and subsequently, insertion of the silicone stent. However, the day after insertion, the silicone stent in the bronchi migrated upward owing to the extrinsic pressure and obstructed the carina. Therefore it had to removed.
Through multidisciplinary cooperation with radiology, we planned to insert a metallic stent. Under wire-guided fluoroscopy, a nitinol metallic stent (Cordis S.M.A.R.T.® CONTROL™ Self-Expanding Nitinol Stent, Florida, United States, right 10 × 40 mm and left 10 × 60 mm) was inserted into both main bronchi (Fig. 3a). The day after nitinol stent insertion, hypoventilation and CO2 retention improved, and the patient was able to remove VV ECMO. During the several invasive procedures, the patient had laceration of the trachea and pneumothorax, but eventually, she could tolerate withdrawal of ventilator support with widened trachea and main bronchi (Fig. 3b, c) and was transferred to local hospital.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd