- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Synergy stent with shorter DAPT is superior to a bare-metal stent in elderly patients
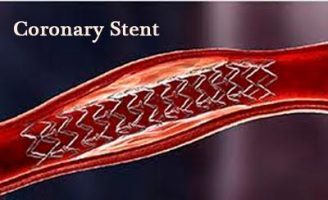
Elderly patients undergoing PCI often receive bare-metal stents (BMS) instead of drug-eluting stents (DES) to shorten the duration of dual antiplatelet therapy (DAPT) and reduce bleeding risk. However, results from the SENIOR trial found that compared with BMS, shorter DAPT combined with the Synergy bioabsorbable polymer DES leads to less adverse events without increasing bleeding risk.
Findings were reported today at the 29th annual Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium. Sponsored by the Cardiovascular Research Foundation (CRF), TCT is the world's premier educational meeting specializing in interventional cardiovascular medicine. The study was also published simultaneously in The Lancet.
Prior to randomization, 1,200 patients aged 75 and older underwent pre-specification of a tailored DAPT strategy: one month for patients with stable angina or silent ischemia, and six months for patients with acute coronary syndrome (including myocardial infarction). Approximately half of patients were in each category based upon clinical presentation. After the intended duration of DAPT was recorded, 596 were assigned to DES and 604 were assigned to BMS. The stent procedure was successful in 98.1% and 97.6% (P=0.561) leading to a complete revascularization at baseline in 85.7% and 86.1% (P=0.860) of DES and BMS-treated patients, respectively. DAPT utilization was similar in both study arms, with approximately half of patients continuing DAPT beyond one month, and only 20% of patients (in both groups) continuing DAPT beyond six months.
The primary endpoint of all-cause mortality, myocardial infarction, stroke, or ischemia-driven target lesion revascularization occurred in 68 patients (11.6%) in the DES group (N=584) and in 98 patients (16.4%) in the BMS group (N=592) (RR 0.71; 95% CI, 0.52-0.94; P=0.0160). This was mainly driven by ischemia driven target-lesion revascularization which was reported in 10 patients (1.7%) in the DES group and in 35 patients (5.9%) in the BMS group (RR 0.29, 95% CI, 0.09-0.49; P=0.0002). Bleeding complications BARC 2-5 (4.5% vs. 5.0%; RR 0.90; 95% CI, 0.51-1.54; P=0.68) and stent thrombosis (0.5% vs. 1.4%, RR 0.38, 95% CI, 0.00-1.48; P=0.1315) rates were low in both groups.
"The elderly represent a fast-growing segment of the population undergoing PCI. They have been poorly represented in prior studies on DES and DAPT duration, so there is no clear recommended PCI strategy for this group," said principal investigator Olivier Varenne, MD, PhD, with the Cardiology Department at Cochin Hospital in Paris, France. "The SENIOR trial shows that among elderly patients who undergo PCI, a DES and a short duration of DAPT is superior to BMS with respect to the occurrence of all-cause mortality, myocardial infarction, stroke, and ischemia-driven target lesion revascularization. Therefore, BMS should no longer be used as a strategy to reduce DAPT duration in these patients."

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd