- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Submandibular Sialadenitis - Standard Treatment Guidelines
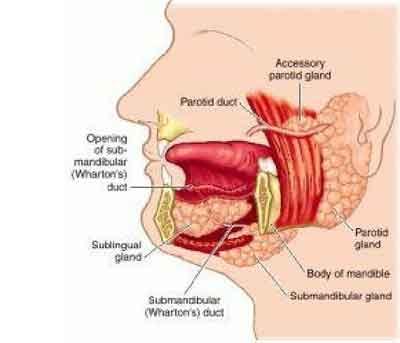
The submandibular gland, along with the parotid and sublingual glands, comprise the major salivary glands. The minor salivary glands are scattered along the upper aerodigestive tract, including the lips, mucosa of the oral cavity, pharynx, and hard palate. The submandibular gland is the second largest (approximate weight, 10 g) of the major salivary glands (the parotid gland is the largest). Anatomically, it is situated in the submandibular triangle of the neck.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Submandibular Sialadenitis. Following are the major recommendations:
Definition :
Sialadenitis of the sub-mandibular gland is a relatively commonly encountered yet infrequently discussed topic. Causes range from simple infection to autoimmune etiologies.
Causes
- Acute sialadenitis
- Chronic sialadenitis
- Sialolithiasis
- Autoimmune sialadenitis
- Sialadenosis
Differential Diagnoses
The differential diagnosis of submandibular sialadenitis and sialadenosis includes the following:
1. Infectious (acute) cause - Bacterial or viral disease
2. Inflammatory cause - Sialolithiasis, radiation-induced disease
3. Autoimmune cause - Sjögren disease, lupus
4. Granulomatous cause - Tuberculosis, tularemia, sarcoidosis, catscratch disease, actinomycosis
5. Drug-related cause - Thiourea
6. Neoplastic (benign) cause - Pleomorphic/monomorphic adenoma, oncocytoma, ductal papilloma, hemangioma, foreign body, ranula, lymphoepithelial cyst
7. Neoplastic (malignant) cause - Adenoid cystic carcinoma, mucoepidermoid carcinoma, adenocarcinoma, undifferentiated carcinoma, malignant oncocytoma, squamous cell carcinoma
8. Endocrine cause - Hypothyroidism, diabetes mellitus
9. Metabolic cause - Vitamin deficiency, cirrhosis, obesity, bulimia, malabsorption
Investigations
1. Ultrasonography
2. Sialography
3. Computed tomography scanning
4. Magnetic resonance imaging
5. Fine-needle aspiration and biopsy
Treatment
One management scheme is as follows:
1. Acute sialadenitis
- Medical management - Hydration, antibiotics (oral versus parenteral), warm compresses and massage, sialogogues
- Surgical management - Consideration of incision and drainage versus excision of the gland in cases refractory to antibiotics, incision and drainage with abscess formation, gland excision in cases of recurrent acute sialadenitis
2. Salivary calculi
- Medical management - Hydration, compression and massage, antibiotics for the infected gland
- Surgical management - Duct cannulation with stone removal, gland excision in recurrent cases
Guidelines by The Ministry of Health and Family Welfare :
Dr J M Hans Ex-HOD Dept. of Otorhinolaryngology Dr.RML Hospital New Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd