- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
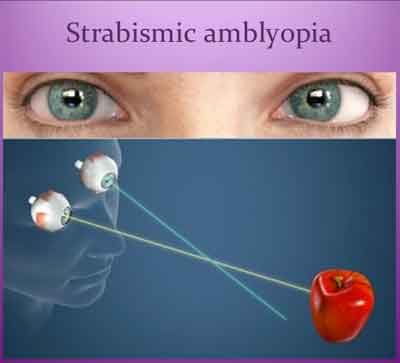
Strabismus and amblyopia: Standard Treatment Guidelines
Strabismus or amblyopia or both together may lead to failure to develop binocular vision which may prevent individual pursuing specific occupations. The associated cosmetic disorder may interfere with social and psychological development with potentially serious effects on individuals. Timely diagnosis and appropriate treatment of children with strabismus and/or amblyopia is likely to reduce the prevalence of persistent amblyopia and ocular misalignment in adults.
Rarely, strabismus and/or amblyopia may be the presenting symptom in children with a serious eye disease or systemic condition (e.g. retinoblastoma or hydrocephalus) when urgent referral to a specialist may be necessary. Amblyopia is the most common visual disability in children. It can present as early as 3 months of age. Its progression and reversibility both are inversely proportional to child’s age. It is commonly unilateral. Nearly all amblyopic visual loss is preventable or reversible with timely detection and appropriate intervention.The Ministry of Health and Family Welfare has issued the Standard Treatment Guidelines for Strabismus and amblyopia. Here are the following recommendations:
I.DEFINITION
Strabismus is a misalignment of the eyes in which the visual axes deviate from bifoveal fixation.
Amblyopia is a unilateral or, less commonly, bilateral reduction of best-corrected visual acuity that cannot only and directly be attributed to the effect of a structural abnormality of the eye or the visual pathways.
For practical purposes, amblyopia is defined as at least 2 Snellen lines difference in visual acuity between the eyes, but amblyopia is truly a spectrum of visual loss, ranging from missing a few letters on the 6/6 (20/20) line to hand motion vision. It is a diagnosis of exclusion. Amblyopia is caused by abnormal visual experience early in life resulting from one of the following:
With timely intervention, the reduction in visual acuity caused by amblyopia can be completely or partially reversed.
II. INCIDENCE OF THE CONDITION IN OUR COUNTRY
There are not many reports available from India about the prevalence of strabismus. One population based study from South India reported the prevalence as 0.43% among children. Another study in North India among school children reported it as 2.5%. The presence of strabismus is not a cosmetic issue only. Its presence says that the child is unable to use both eyes together and there could be some other ocular problem that is undetected.
Different studies from developed countries on amblyopia have an estimated prevalence in childhood of 1.2% to 4.4% depending on the defining criteria.
III. DIFFERENTIAL DIAGNOSIS
Strabismus
Amblyopia
IV. PREVENTION AND COUNSELING
Recent studies have shown that early detection and treatment of amblyopia are highly cost effective when compared with other interventions in health care. The earlier amblyopia is detected and properly treated, the higher the likelihood of visual acuity recovery. Starting treatment at a young age also may increase the likelihood of compliance and the rate of vision recovery. The Amblyopia Treatment Study demonstrated that more than 75% of amblyopic children younger than 7 years can have significant improvement in the amblyopic eye (to 20/30 or better) as the result of treatment. The purpose of periodic eye and vision screening is to detect pediatric eye disorders, especially amblyopia, at a sufficiently early age to allow effective treatment. All children should undergo eye and vision screening, because screening is most effective when performed periodically throughout childhood.
In addition, children with risk factors for amblyopia should have a comprehensive ophthalmic evaluation. Some risk factors include family history of amblyopia or strabismus, childhood cataract or glaucoma, premature birth of less than 30-week gestation or 1,500 grams, and delayed visual or neurologic maturation of unclear etiology. Reduction or prevention of risk factors such as premature birth and detrimental prenatal environmental influences such as alcohol abuse and smoking can result in a decrease in the incidence of amblyopia.
V. OPTIMAL DIAGNOSTIC CRITERIA, INVESTIGATIONS, TREATMENT & REFERRAL CRITERIA
*Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited
a) Clinical Diagnosis:
The initial strabismus and amblyopia evaluation (history and physical examination) includes all components of the comprehensive pediatric ophthalmic evaluation, with special attention to the potential risk factors for amblyopia, such as a positive family history for strabismus, amblyopia, or media opacity.
The examination of a patient who has childhood-onset strabismus includes all components of the comprehensive pediatric or adult ophthalmic evaluation in addition to the sensory, motor, refractive, and accommodative functions.
History
Systemic history: birth weight, prenatal (e.g., alcohol, tobacco, and drug use during pregnancy), and perinatal history (e.g. birth asphyxia, trauma) that may be pertinent, past hospitalizations and operations, general health and development.
Examination
The eye examination consists of an assessment of the physiological function and the anatomic status of the eye and visual system. Documentation of the child’s level of cooperation with the examination can be useful in interpreting the results and in making comparisons among the examinations over time. In general, the examination may include the following elements:
Extraocular muscle function (ductions and versions including incomitance, such as A and V patterns)
Assessment of Visual Acuity and Fixation Pattern
The method of evaluating visual acuity varies according to the child’s age and level of cooperation. Preverbal children should be checked for objection to cover and the presence of a fixation preference. When possible, monocular distance visual acuity should be determined utilizing a recognized optotype, such as the tumbling-E, Lea figures, or Snellen letters.
Anomalous head posture is suggestive of peeking around the occluder. An occlusive patch over the non-tested eye can distinguish between peeking and possible eccentric fixation. Monocular visual acuity testing for patients with nystagmus may require blurring of the contralateral eye with a high plus lens (+4.00 D to +5.00 D). Binocular and monocular testing also should be performed for patients with nystagmus.
Testing visual acuity with isolated targets (figures or letters) is the quickest way to assess the vision in preverbal children, but it does lead to falsely elevated visual acuities. Isolated acuities should be compared with visual acuities taken with linear targets or crowding bars. The difference between linear and isolated acuities should be noted at each visit, if possible. This difference is a way of quantifying the depth of amblyopia from visit to visit.
Under ideal circumstances, visual acuity testing conditions should be standardized in each examination room and at each visit, so that the same viewing distance and lighting conditions are used. Some children are more amenable to testing at shorter distances.
Young children sometimes benefit from shorter testing distances, especially when a visual or attention deficit is suspected. The testing distance, type of optotype, and whether the optotype is presented a line at a time or isolated, should be documented. Patients should be encouraged to learn optotype-equivalent tests at the earliest possible age.
Ocular Alignment and Motility
Ocular alignment is assessed by using the corneal light reflection, the binocular red reflex (Brückner) test, or the cover test. Cover/uncover and alternate cover tests in primary gaze at distance and near accommodative targets are utilized when feasible; these tests require the patient's cooperation and interaction with the examiner in addition to sufficient vision to fixate on the target. Ocular versions and ductions should be tested even in the young infant. In the inattentive or uncooperative patient, eye movements may be tested using the oculocephalic rotations maneuver (doll’s head) or assessed by spontaneous eye movements. Evaluating oblique muscle function in young children is important when examining a child with strabismus, but it may be difficult. When strabismus is suspected or revealed, a strabismus evaluation is warranted).
Red Reflex / Binocular Red Reflex (Brückner) Test
The red reflex and/or binocular red reflex test should be performed to identify opacities of the ocular media.
The red reflex of each eye is assessed by looking at each eye with a direct ophthalmoscope from a distance of about 18 inches. The examiner should answer three questions:
1. Is there a red reflex from each eye?
2. Are the red reflexes from each eye symmetrical?
3. Is the quality of the red reflex normal for the individual child (taking into account skin tone and race or ethnicity)?
The binocular red reflex (Brückner) test allows an assessment of the clarity of the visual axis and an indirect assessment of ocular alignment as well as large and/or asymmetric refractive errors. The binocular red reflex test is performed in a dimly lit room with the examiner at a distance of about 30 inches (0.75 meter) from the child. The examiner overlaps both pupils simultaneously, creating a binocular red reflex with the largest circular light of a direct ophthalmoscope set to focus on the ocular surface, usually at zero. The examiner then assesses the quality of the redness seen within the child’s pupils. Normally, the red reflex from each eye should be of the same color and brightness.
Abnormalities include asymmetric reflexes when one reflex is duller or a different color, a white reflex, a partially or totally obscured reflex, or crescents present in the reflex.
Extraocular Muscle Function
Versions and ductions should be evaluated and any over- or underactions of extraocular muscles assessed and recorded. Inferior oblique muscle dysfunction, A or V patterns, or dissociated vertical or horizontal deviations may develop over time. The examiner should note any limitations in versions or ductions. The oculocephalic rotations maneuver (doll’s head) is particularly valuable in infants and young children and often reveals clinically normal ductions that cannot otherwise be documented, even with patch testing.
Detection of Nystagmus
Nystagmus in the patient with esotropia may be manifest or latent. Manifest nystagmus is constantly present and may be horizontal, vertical, or torsional. It is typically symmetrical, although it may vary in magnitude, speed, and wave form, depending on the direction of gaze and other specific viewing conditions. Latent nystagmus (sometimes called occlusion nystagmus) is conjugate, predominantly horizontal, jerk oscillations of the eyes that are produced or exacerbated by monocular viewing. It is characterized by a slow drift away from the fixating eye, with rhythmic jerk redress movements to re-establish central fixation. The nystagmus is described as latent because it is typically perceptible or accentuated when one eye is occluded. Both manifest and latent nystagmus may coexist in the same patient.
Sensory Testing
The binocular sensory status should be assessed when feasible using Worth 4-dot testing and stereoacuity tests. Reliable data may be difficult to obtain in younger children.In the older strabismic (especially esotropic) patient, more detailed sensory testing is occasionally useful, especially if there is a history of diplopia. An orthoptic evaluation may be useful to further define the sensory status of the child.
Pupil Examination
Even in small infants, the pupils should be assessed for direct and consensual response to light and for the presence of a relative afferent defect. This can be done with a penlight, a direct ophthalmoscope, or a transilluminator. Pupil evaluation in infants and children may be difficult due to active hippus or shift in the patient’s fixation and accommodative status. In general, amblyopia is not associated with a detectable afferent pupillary defect. If an afferent pupillary defect is present, the examiner should thoroughly review etiologic causes for asymmetric optic nerve function rather than attribute the finding to amblyopia.
External Examination
External examination involves assessment of the eyelids, eyelashes, lacrimal apparatus, and orbit.The anatomy of the face (including the lids, interocular distance, and presence or absence of epicanthal folds), orbital rim, and presence of oculofacial anomalies should be noted. The position of the head and face (including head tilt or turn) should be noted. Children with prominent epicanthal folds and normal ocular alignment may appear to have an esotropia (pseudo-esotropia). Distinctive features unusual for the family may suggest the presence of a congenital anomaly and merit an assessment of other physical abnormalities (e.g., ears, hands).
Anterior Segment Examination
To evaluate further opacities of the ocular media, the cornea, anterior chamber, iris, and lens should be evaluated with slit-lamp biomicroscopy if possible Slit-lamp biomicroscopic evaluation is easily performed for older children or for younger children who are cooperative. In infants and young children, a hand-held slit-lamp biomicroscope may be helpful. Some children may need to be restrained, sedated, or undergo an eye examination under general anesthesia when apparent abnormalities warrant a detailed examination.
Cycloplegic Retinoscopy/Refraction
Determination of refractive errors is important in the diagnosis and treatment of amblyopia or strabismus. Patients should receive an accurate cycloplegic refraction either by retinoscopy or by subjective refraction. Prior to cycloplegia, dynamic retinoscopy provides a rapid assessment of accommodative function and may be helpful in evaluating a child with high hyperopia or possible accommodative insufficiency.
Cycloplegia is necessary for accurate refraction in children. Cyclopentolate is useful because it has a rapid onset and produces cycloplegia that approximates the effect of topical ophthalmic atropine but with a shorter duration of action. Cyclopentolate 1% is more frequently used; cyclopentolate 2% is also available. The strength of cyclopentolate should be determined based on the child's weight, iris coloration, and dilation history. In eyes with heavily pigmented irides, adjunctive agents such as tropicamide and/or phenylephrine hydrochloride may be necessary to achieve adequate dilation. In rare cases, topical ophthalmic atropine may be necessary to achieve maximal cycloplegia. The use of topical anesthetic prior to the cycloplegic makes the cycloplegic sting less and promotes its penetration into the eye.
Funduscopic Examination
Posterior segment structures should be examined, preferably with an indirect ophthalmoscope. The optic disc, macula, retina, vessels, and the choroid of the posterior regions should be examined Examination of the peripheral retinal and scleral indentation, if indicated, may require sedation or general anesthesia (e.g., evaluation for retinoblastoma).
Binocularity / Stereoacuity Testing
Testing for binocular fusion (e.g., Worth 4-dot test) or the presence of stereopsis (e.g., Random-Dot E test or Stereo Fly test) may be useful in detecting ocular misalignment or
amblyopia. Fusion and stereoacuity testing at distance (20 feet or 6 meters) as well as near (13 inches or 0.33 meter) may also be helpful.
b) Investigations:
Strabismus and Amblyopia are mostly clinically diagnosed and treatment is planned based on routine examination and orthoptic check up. B scan ultrasonogram may be needed for associated media opacity and intra ocular tumors. Rarely CT scan and Electrophysiological tests are needed for assisting diagnosis.
c) Treatment:
Amblyopia:
Choice of Therapy
The following therapies are used alone or in combination as required to achieve the therapeutic goal.
Strabismus:
Ocular alignment should be established as soon as possible, especially in young children, to maximize binocularity, prevent or facilitate treatment of amblyopia, and normalize appearance. In almost all cases, clinically important refractive errors should be corrected. Amblyopia treatment is usually started before surgery, because this may reduce the angle of strabismus or increase the likelihood of good postoperative binocularity.
The following treatment modalities are used alone or in combination as required to achieve the therapeutic goal:
Prism therapy
Treatment plans are formulated in consultation with the patient and parents. The plans should be responsive to their expectations and preferences, including the family’s perception of the existing alignment, which may differ among ophthalmologist’s, and what they hope to achieve with treatment. It is important that the family and ophthalmologist agree on the goals of treatment before surgery is performed. A particularly challenging situation can arise when the surgical intervention might worsen the appearance of the child. In patients for whom the potential for binocularity is poor, surgery to normalize appearance is still appropriate treatment.
The amount of surgery and the choice of surgical technique may vary (e.g., methods of suture placement in the muscle and sclera, or measurement of recession or resection). Although two-muscle surgery is most frequently performed, sometimes three- or four-horizontal-muscle surgery may be required for large-angle deviations.
Results may be similar with different procedures; one method may be chosen over another on the basis of preoperative diagnosis, angle of deviation, technical ease, anatomical exposure, the need for an assistant, presence of scar tissue, and other factors such as physician preference and experience. Bilateral medial rectus muscle recessions are commonly performed as the initial surgical procedure. Most surgeons prefer uniocular surgery (single-muscle recession or recession/resection) for patients with irreversible amblyopia or substantially reduced vision in one eye on an anatomic basis. Operating on both eyes may be preferable in specific clinical circumstances, such as V pattern esotropia with inferior oblique-muscle overaction or null-point nystagmus with compensatory face turn.
Standard Operating procedure
a. In Patient
b. Out Patient
Non surgical treatment
Pre operative investigations
Follow up
c. Day Care
If patients prefer and are able to reach the clinic easily if required
d) Referral criteria:
*Situation 2: At Super Specialty Facility in Metro location where higher-end technology is available
a) Clinical Diagnosis: Same as situation 1 plus better orthoptic examination.
b) Investigations: Same as situation 1. In addition, USG B Scan and electrophysiological tests are done if needed. Paediatric and neurological consultation back up and facility for relevant systemic investigations is required in indicated patients.
c) Treatment:
Same as situation1. In addition, the ophthalmologist should be able to take up complex surgeries. Interdiscipinary referral between the anterior and posterior segment specialists is required in certain cases. Low vision aids may be required in some individuals
Standard Operating procedure
a. In Patient
b. Out Patient
Non surgical treatment; Pre operative investigations; Follow up
c. Day Care
If patients prefer and are able to reach the clinic easily if required
d) Referral criteria:
Does not apply
VI. WHO DOES WHAT? and TIMELINES
a. Doctor
Patient History is taken and a Clinical Examination performed
b. Nurse / Technician
Guideline of Ministry of Health & Family Welfare Govt. of India.
Group Head Coordinator of Development Team
Dr. Venkatesh Prajna Chief- Dept of Medical Education,
Aravind Eye Hospitals, Madurai
Rarely, strabismus and/or amblyopia may be the presenting symptom in children with a serious eye disease or systemic condition (e.g. retinoblastoma or hydrocephalus) when urgent referral to a specialist may be necessary. Amblyopia is the most common visual disability in children. It can present as early as 3 months of age. Its progression and reversibility both are inversely proportional to child’s age. It is commonly unilateral. Nearly all amblyopic visual loss is preventable or reversible with timely detection and appropriate intervention.The Ministry of Health and Family Welfare has issued the Standard Treatment Guidelines for Strabismus and amblyopia. Here are the following recommendations:
I.DEFINITION
Strabismus is a misalignment of the eyes in which the visual axes deviate from bifoveal fixation.
Amblyopia is a unilateral or, less commonly, bilateral reduction of best-corrected visual acuity that cannot only and directly be attributed to the effect of a structural abnormality of the eye or the visual pathways.
For practical purposes, amblyopia is defined as at least 2 Snellen lines difference in visual acuity between the eyes, but amblyopia is truly a spectrum of visual loss, ranging from missing a few letters on the 6/6 (20/20) line to hand motion vision. It is a diagnosis of exclusion. Amblyopia is caused by abnormal visual experience early in life resulting from one of the following:
- Strabismus
- Anisometropia or high bilateral refractive errors (isometropia)
- Visual deprivation
With timely intervention, the reduction in visual acuity caused by amblyopia can be completely or partially reversed.
II. INCIDENCE OF THE CONDITION IN OUR COUNTRY
There are not many reports available from India about the prevalence of strabismus. One population based study from South India reported the prevalence as 0.43% among children. Another study in North India among school children reported it as 2.5%. The presence of strabismus is not a cosmetic issue only. Its presence says that the child is unable to use both eyes together and there could be some other ocular problem that is undetected.
Different studies from developed countries on amblyopia have an estimated prevalence in childhood of 1.2% to 4.4% depending on the defining criteria.
III. DIFFERENTIAL DIAGNOSIS
Strabismus
- Pseudostrabismus
- Nystagmus
- Facial asymmetry
Amblyopia
- Nutritional/Toxic optic neuropathy
- Malingering
- Cortical blindness
IV. PREVENTION AND COUNSELING
Recent studies have shown that early detection and treatment of amblyopia are highly cost effective when compared with other interventions in health care. The earlier amblyopia is detected and properly treated, the higher the likelihood of visual acuity recovery. Starting treatment at a young age also may increase the likelihood of compliance and the rate of vision recovery. The Amblyopia Treatment Study demonstrated that more than 75% of amblyopic children younger than 7 years can have significant improvement in the amblyopic eye (to 20/30 or better) as the result of treatment. The purpose of periodic eye and vision screening is to detect pediatric eye disorders, especially amblyopia, at a sufficiently early age to allow effective treatment. All children should undergo eye and vision screening, because screening is most effective when performed periodically throughout childhood.
In addition, children with risk factors for amblyopia should have a comprehensive ophthalmic evaluation. Some risk factors include family history of amblyopia or strabismus, childhood cataract or glaucoma, premature birth of less than 30-week gestation or 1,500 grams, and delayed visual or neurologic maturation of unclear etiology. Reduction or prevention of risk factors such as premature birth and detrimental prenatal environmental influences such as alcohol abuse and smoking can result in a decrease in the incidence of amblyopia.
V. OPTIMAL DIAGNOSTIC CRITERIA, INVESTIGATIONS, TREATMENT & REFERRAL CRITERIA
*Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited
a) Clinical Diagnosis:
The initial strabismus and amblyopia evaluation (history and physical examination) includes all components of the comprehensive pediatric ophthalmic evaluation, with special attention to the potential risk factors for amblyopia, such as a positive family history for strabismus, amblyopia, or media opacity.
The examination of a patient who has childhood-onset strabismus includes all components of the comprehensive pediatric or adult ophthalmic evaluation in addition to the sensory, motor, refractive, and accommodative functions.
History
Although a thorough history generally includes the following items, the exact composition varies with the patient's particular problems and needs:
- The chief complaint and reason for the eye evaluation
- Current eye problems
- Ocular history, including prior eye problems, diseases, diagnoses, and treatments
Systemic history: birth weight, prenatal (e.g., alcohol, tobacco, and drug use during pregnancy), and perinatal history (e.g. birth asphyxia, trauma) that may be pertinent, past hospitalizations and operations, general health and development.
- Pertinent review of systems, including history of head trauma and relevant systemic diseases
- Current medications and allergies
- Family history of eye conditions and relevant systemic diseases
- Review of systems.
Examination
The eye examination consists of an assessment of the physiological function and the anatomic status of the eye and visual system. Documentation of the child’s level of cooperation with the examination can be useful in interpreting the results and in making comparisons among the examinations over time. In general, the examination may include the following elements:
- Assessment of visual acuity and fixation pattern
- Ocular alignment and motility for near and distance
Extraocular muscle function (ductions and versions including incomitance, such as A and V patterns)
- Detection of nystagmus
- Sensory testing
- Red reflex or binocular red reflex (Brückner) test
- Pupil examination
- External examination
- Anterior segment examination
- Cycloplegic retinoscopy/refraction
- Funduscopic examination
- Binocularity/stereoacuity testing
Assessment of Visual Acuity and Fixation Pattern
The method of evaluating visual acuity varies according to the child’s age and level of cooperation. Preverbal children should be checked for objection to cover and the presence of a fixation preference. When possible, monocular distance visual acuity should be determined utilizing a recognized optotype, such as the tumbling-E, Lea figures, or Snellen letters.
Anomalous head posture is suggestive of peeking around the occluder. An occlusive patch over the non-tested eye can distinguish between peeking and possible eccentric fixation. Monocular visual acuity testing for patients with nystagmus may require blurring of the contralateral eye with a high plus lens (+4.00 D to +5.00 D). Binocular and monocular testing also should be performed for patients with nystagmus.
Testing visual acuity with isolated targets (figures or letters) is the quickest way to assess the vision in preverbal children, but it does lead to falsely elevated visual acuities. Isolated acuities should be compared with visual acuities taken with linear targets or crowding bars. The difference between linear and isolated acuities should be noted at each visit, if possible. This difference is a way of quantifying the depth of amblyopia from visit to visit.
Under ideal circumstances, visual acuity testing conditions should be standardized in each examination room and at each visit, so that the same viewing distance and lighting conditions are used. Some children are more amenable to testing at shorter distances.
Young children sometimes benefit from shorter testing distances, especially when a visual or attention deficit is suspected. The testing distance, type of optotype, and whether the optotype is presented a line at a time or isolated, should be documented. Patients should be encouraged to learn optotype-equivalent tests at the earliest possible age.
Ocular Alignment and Motility
Ocular alignment is assessed by using the corneal light reflection, the binocular red reflex (Brückner) test, or the cover test. Cover/uncover and alternate cover tests in primary gaze at distance and near accommodative targets are utilized when feasible; these tests require the patient's cooperation and interaction with the examiner in addition to sufficient vision to fixate on the target. Ocular versions and ductions should be tested even in the young infant. In the inattentive or uncooperative patient, eye movements may be tested using the oculocephalic rotations maneuver (doll’s head) or assessed by spontaneous eye movements. Evaluating oblique muscle function in young children is important when examining a child with strabismus, but it may be difficult. When strabismus is suspected or revealed, a strabismus evaluation is warranted).
Red Reflex / Binocular Red Reflex (Brückner) Test
The red reflex and/or binocular red reflex test should be performed to identify opacities of the ocular media.
The red reflex of each eye is assessed by looking at each eye with a direct ophthalmoscope from a distance of about 18 inches. The examiner should answer three questions:
1. Is there a red reflex from each eye?
2. Are the red reflexes from each eye symmetrical?
3. Is the quality of the red reflex normal for the individual child (taking into account skin tone and race or ethnicity)?
The binocular red reflex (Brückner) test allows an assessment of the clarity of the visual axis and an indirect assessment of ocular alignment as well as large and/or asymmetric refractive errors. The binocular red reflex test is performed in a dimly lit room with the examiner at a distance of about 30 inches (0.75 meter) from the child. The examiner overlaps both pupils simultaneously, creating a binocular red reflex with the largest circular light of a direct ophthalmoscope set to focus on the ocular surface, usually at zero. The examiner then assesses the quality of the redness seen within the child’s pupils. Normally, the red reflex from each eye should be of the same color and brightness.
Abnormalities include asymmetric reflexes when one reflex is duller or a different color, a white reflex, a partially or totally obscured reflex, or crescents present in the reflex.
Extraocular Muscle Function
Versions and ductions should be evaluated and any over- or underactions of extraocular muscles assessed and recorded. Inferior oblique muscle dysfunction, A or V patterns, or dissociated vertical or horizontal deviations may develop over time. The examiner should note any limitations in versions or ductions. The oculocephalic rotations maneuver (doll’s head) is particularly valuable in infants and young children and often reveals clinically normal ductions that cannot otherwise be documented, even with patch testing.
Detection of Nystagmus
Nystagmus in the patient with esotropia may be manifest or latent. Manifest nystagmus is constantly present and may be horizontal, vertical, or torsional. It is typically symmetrical, although it may vary in magnitude, speed, and wave form, depending on the direction of gaze and other specific viewing conditions. Latent nystagmus (sometimes called occlusion nystagmus) is conjugate, predominantly horizontal, jerk oscillations of the eyes that are produced or exacerbated by monocular viewing. It is characterized by a slow drift away from the fixating eye, with rhythmic jerk redress movements to re-establish central fixation. The nystagmus is described as latent because it is typically perceptible or accentuated when one eye is occluded. Both manifest and latent nystagmus may coexist in the same patient.
Sensory Testing
The binocular sensory status should be assessed when feasible using Worth 4-dot testing and stereoacuity tests. Reliable data may be difficult to obtain in younger children.In the older strabismic (especially esotropic) patient, more detailed sensory testing is occasionally useful, especially if there is a history of diplopia. An orthoptic evaluation may be useful to further define the sensory status of the child.
Pupil Examination
Even in small infants, the pupils should be assessed for direct and consensual response to light and for the presence of a relative afferent defect. This can be done with a penlight, a direct ophthalmoscope, or a transilluminator. Pupil evaluation in infants and children may be difficult due to active hippus or shift in the patient’s fixation and accommodative status. In general, amblyopia is not associated with a detectable afferent pupillary defect. If an afferent pupillary defect is present, the examiner should thoroughly review etiologic causes for asymmetric optic nerve function rather than attribute the finding to amblyopia.
External Examination
External examination involves assessment of the eyelids, eyelashes, lacrimal apparatus, and orbit.The anatomy of the face (including the lids, interocular distance, and presence or absence of epicanthal folds), orbital rim, and presence of oculofacial anomalies should be noted. The position of the head and face (including head tilt or turn) should be noted. Children with prominent epicanthal folds and normal ocular alignment may appear to have an esotropia (pseudo-esotropia). Distinctive features unusual for the family may suggest the presence of a congenital anomaly and merit an assessment of other physical abnormalities (e.g., ears, hands).
Anterior Segment Examination
To evaluate further opacities of the ocular media, the cornea, anterior chamber, iris, and lens should be evaluated with slit-lamp biomicroscopy if possible Slit-lamp biomicroscopic evaluation is easily performed for older children or for younger children who are cooperative. In infants and young children, a hand-held slit-lamp biomicroscope may be helpful. Some children may need to be restrained, sedated, or undergo an eye examination under general anesthesia when apparent abnormalities warrant a detailed examination.
Cycloplegic Retinoscopy/Refraction
Determination of refractive errors is important in the diagnosis and treatment of amblyopia or strabismus. Patients should receive an accurate cycloplegic refraction either by retinoscopy or by subjective refraction. Prior to cycloplegia, dynamic retinoscopy provides a rapid assessment of accommodative function and may be helpful in evaluating a child with high hyperopia or possible accommodative insufficiency.
Cycloplegia is necessary for accurate refraction in children. Cyclopentolate is useful because it has a rapid onset and produces cycloplegia that approximates the effect of topical ophthalmic atropine but with a shorter duration of action. Cyclopentolate 1% is more frequently used; cyclopentolate 2% is also available. The strength of cyclopentolate should be determined based on the child's weight, iris coloration, and dilation history. In eyes with heavily pigmented irides, adjunctive agents such as tropicamide and/or phenylephrine hydrochloride may be necessary to achieve adequate dilation. In rare cases, topical ophthalmic atropine may be necessary to achieve maximal cycloplegia. The use of topical anesthetic prior to the cycloplegic makes the cycloplegic sting less and promotes its penetration into the eye.
Funduscopic Examination
Posterior segment structures should be examined, preferably with an indirect ophthalmoscope. The optic disc, macula, retina, vessels, and the choroid of the posterior regions should be examined Examination of the peripheral retinal and scleral indentation, if indicated, may require sedation or general anesthesia (e.g., evaluation for retinoblastoma).
Binocularity / Stereoacuity Testing
Testing for binocular fusion (e.g., Worth 4-dot test) or the presence of stereopsis (e.g., Random-Dot E test or Stereo Fly test) may be useful in detecting ocular misalignment or
amblyopia. Fusion and stereoacuity testing at distance (20 feet or 6 meters) as well as near (13 inches or 0.33 meter) may also be helpful.
b) Investigations:
Strabismus and Amblyopia are mostly clinically diagnosed and treatment is planned based on routine examination and orthoptic check up. B scan ultrasonogram may be needed for associated media opacity and intra ocular tumors. Rarely CT scan and Electrophysiological tests are needed for assisting diagnosis.
c) Treatment:
Amblyopia:
Choice of Therapy
The following therapies are used alone or in combination as required to achieve the therapeutic goal.
- Optical correction: The amblyopic eye must have the most accurate optical correction possible. This should occur prior to any occlusion therapy because vision may improve with spectacles alone. Full cycloplegic refraction should be given to patients with accommodative esotropia and amblyopia. In other patients, a prescription less than the full plus measurement that was refracted may be prescribed given that the decrease in plus is symmetric between the two eyes. Because accommodative amplitude is believed to be decreased in amblyopic eyes, one needs to be cautious about cutting back too much on the amount of plus. Refractive correction alone has been shown to improve amblyopia in up to 77% of patients.
- Occlusion: Patching may be full-time or part-time. Standard teaching has been that children need to be observed at intervals of 1 week per year of age, if undergoing full-time occlusion to avoid occlusion amblyopia in the sound eye . In addition to adhesive patches, opaque contact lenses, occluders mounted on spectacles, and adhesive tape on glasses have been used.
- Penalization: Penalization therapy was reserved for children who would not wear a patch or in whom compliance was an issue. The Amblyopia Treatment Studies, however, have demonstrated that atropine penalization in patients with moderate amblyopia (defined by the study as visual acuity better than 20/100) is as effective as patching. The Amblyopia Treatment Studies were performed in children aged 3-7 year.
- Surgery to treat the cause of the amblyopia
In general, occlusive adhesive patches should be used during the initial therapy in many cases of amblyopia; however, in mild to moderate amblyopia, penalization with atropine drops has been shown to be an effective alternative.
Strabismus:
Ocular alignment should be established as soon as possible, especially in young children, to maximize binocularity, prevent or facilitate treatment of amblyopia, and normalize appearance. In almost all cases, clinically important refractive errors should be corrected. Amblyopia treatment is usually started before surgery, because this may reduce the angle of strabismus or increase the likelihood of good postoperative binocularity.
The following treatment modalities are used alone or in combination as required to achieve the therapeutic goal:
- Correction of refractive errors
- Bifocals
- Miotics
Prism therapy
- Amblyopia treatment
- Extraocular muscle surgery: Except few conditions (like, accommodative esotropia), strabismus is corrected with surgery.
Treatment plans are formulated in consultation with the patient and parents. The plans should be responsive to their expectations and preferences, including the family’s perception of the existing alignment, which may differ among ophthalmologist’s, and what they hope to achieve with treatment. It is important that the family and ophthalmologist agree on the goals of treatment before surgery is performed. A particularly challenging situation can arise when the surgical intervention might worsen the appearance of the child. In patients for whom the potential for binocularity is poor, surgery to normalize appearance is still appropriate treatment.
The amount of surgery and the choice of surgical technique may vary (e.g., methods of suture placement in the muscle and sclera, or measurement of recession or resection). Although two-muscle surgery is most frequently performed, sometimes three- or four-horizontal-muscle surgery may be required for large-angle deviations.
Results may be similar with different procedures; one method may be chosen over another on the basis of preoperative diagnosis, angle of deviation, technical ease, anatomical exposure, the need for an assistant, presence of scar tissue, and other factors such as physician preference and experience. Bilateral medial rectus muscle recessions are commonly performed as the initial surgical procedure. Most surgeons prefer uniocular surgery (single-muscle recession or recession/resection) for patients with irreversible amblyopia or substantially reduced vision in one eye on an anatomic basis. Operating on both eyes may be preferable in specific clinical circumstances, such as V pattern esotropia with inferior oblique-muscle overaction or null-point nystagmus with compensatory face turn.
Standard Operating procedure
a. In Patient
- Patients preferring hospital stay for surgery because of distance and better care
If decided by the anaesthesiologist - Patients needing some adjustment of sutures on the next day
- Patients with post operative complications that need institutional care
b. Out Patient
Non surgical treatment
Pre operative investigations
Follow up
c. Day Care
If patients prefer and are able to reach the clinic easily if required
d) Referral criteria:
- Cases needing specialized investigations (e.g USG B-Scan, Electrophysiological tests)
- Cases not manageable by the facilities available .
- Seeking second opinion
- Complications needing specialized intervention.
- Complex cases like torsional deviation, DVD, Duanes retraction syndrome etc.,needs referral
*Situation 2: At Super Specialty Facility in Metro location where higher-end technology is available
a) Clinical Diagnosis: Same as situation 1 plus better orthoptic examination.
b) Investigations: Same as situation 1. In addition, USG B Scan and electrophysiological tests are done if needed. Paediatric and neurological consultation back up and facility for relevant systemic investigations is required in indicated patients.
c) Treatment:
Same as situation1. In addition, the ophthalmologist should be able to take up complex surgeries. Interdiscipinary referral between the anterior and posterior segment specialists is required in certain cases. Low vision aids may be required in some individuals
Standard Operating procedure
a. In Patient
- Patients preferring hospital stay for surgery because of distance and better care
If decided by the Anaesthesiologist - Patients needing some adjustment of sutures on the next day
- Patients with post operative complications that need institutional care
b. Out Patient
Non surgical treatment; Pre operative investigations; Follow up
c. Day Care
If patients prefer and are able to reach the clinic easily if required
d) Referral criteria:
Does not apply
VI. WHO DOES WHAT? and TIMELINES
a. Doctor
Patient History is taken and a Clinical Examination performed
- Documenting the medical record
- Plan treatment guidelines and counsel patients
- Perform surgery. Explain and assure patients if complications occur.
- Follow up
- Referral in needed.
- Monitoring the functional improvement and if needed guide parents in rehabilitation
b. Nurse / Technician
- Receive the patients and assist in clinical examination
- Refraction
- Orthoptic check up
- Counseling whenever patients/ parents
- Prepare the patients for surgery
- To monitor the patients who are admitted regarding pre and post operative care
- To maintain separate inpatient and outpatient record
- To maintain lab reports
- Explain discharge advice to patients
- Proactively ensure follow up through counseling.
| Situation | HUMAN RESOURCES | INVESTIGATIONS | DRUGS & CONSUMABLES | EQUIPMENT |
| 1] Secondary level | 1)Ophthalmologist - 1 2)OP Nurse – 1 3)Ophthalmic Assistant / 4)Optometrist trained in orthoptics 1 | 1)Refraction 2)Orthoptic check up | 1)Cycloplegics 2)Local Anaesthetics 3)Antibiotics eye drops | 1)Torch light 2)Trial set 3)Prism set 4)Retinoscope 5)Slit lamp - biomicroscope 6)Direct Ophthalmoscope 7)+90 D lens 8)Indirect Ophthalmoscope with +20 D lens |
| 2] Tertiary level | 1)Experienced Ophthalmologist - 1 2)OP Nurse – 1 3)Ophthalmic Assistant / 4)Optometrist -1 5)Orthoptist -1 6)Anaesthesiologist -1 7)Assisting Nurse -1 8) Counsellor - 1 | 1)Refraction 2)Strabismus assessment 3)Biometry 4)USG B- Scan 5)Examination under short GA | 1)Local anaesthetics 2)Antibiotics eye drops 3)Mydriatics 4)General 5)Anaesthetic medications | 1)Torch light 2)Trial set 3)Prism set 4)RAF Rule 5)Synoptophore 6)Hess’s screen 7)Retinoscope 8)Slit lamp - biomicroscope 9)Direct Ophthalmoscope 10)+90 D lens 11)Indirect Ophthalmoscope 12)Applanation tonometer (Perkin’s) 13)Gonioscope with +20 D lens 14)A-Scan Keratometer 15)USG B- Scan 16)Boyle’s apparatus 17)Pulse oxymeter |
Guideline of Ministry of Health & Family Welfare Govt. of India.
Group Head Coordinator of Development Team
Dr. Venkatesh Prajna Chief- Dept of Medical Education,
Aravind Eye Hospitals, Madurai
Cortical blindnessFacial asymmetryMalingeringNutritional/Toxic optic neuropathyNystagmusPseudostrabismusStrabismusSTRABISMUS AND AMBLYOPIA
Next Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd