- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Standard Treatment Guidelines For Ectopic Pregnancy
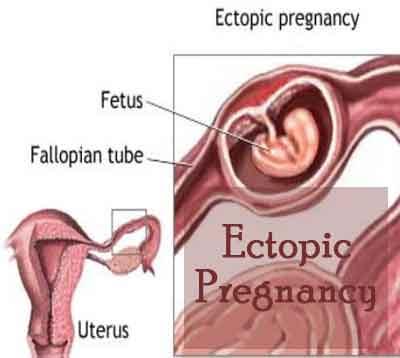
When implantation of the embryo occurs outside the uterine cavity is called ectopic pregnancy. Common site of implantation is in the fallopian tube. The issue comes across in 1-3% of pregnancies in India
The risk of death from an undiagnosed ectopic pregnancy is greater than that of an induced abortion or delivery. Therefore slogan is “If you think ectopic then only you can diagnose ectopic”. Earlier the diagnosis, better is the prognosis with conservation of the reproductive capacity. Chances of a subsequent successful pregnancy are reduced in these women.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Ectopic Pregnancy. Following are the major recommendations :
Risk factors for ectopic pregnancy
PID
Endometriosis
IUCD use
Progesterone only contraceptive pill use
Pregnancy after tubal ligation, tubal surgery
ovulation induction and assisted reproduction techniques,
I Case definition:
For both situations of care (mentioned below) Implantation of the embryo anywhere else other than the endometrial lining of the uterine cavity is an ectopic pregnancy.
II. Incidence of the condition in our country:
1 to 3% of all pregnancies.
III. Differential diagnosis:
Very early intrauterine pregnancy Heterotopic pregnancy
IV Optimal diagnostic criteria, investigations, treatment and referral criteria
Situation- At Secondary Hospital/ Non Metro situation: Optimal Standards of treatment in Situations where technology and resources are limited.
a) Clinical Diagnosis:
Presentation could be diverse depends on whether rupture has occurred. The reproductive age group woman may present with amenorrhoea, bleeding pv, pain abdomen, sometimes with shock due to rupture.
b) Investigations:
1. A urine pregnancy test should be positive
2. Ultrasound abdominal/ vaginal- thickened echogenic endometrium, absent intrauterine gestational sac, sometimes a pseudosac, fluid in the culde sac, occasionally haematosalpinx, adnexal mass or a tubal ring representing the gestational sac.
3. Culdocentesis if ultrasound facility is not available
4. Blood grouping crossmatching and reservation
5. Histopathological examination of the operative specimen to confirm diagnosis.
c) Treatment:
The standard aim of care is to control the bleeding and remove the ectopic pregnancy.
Start an IV line, arrange for blood transfusion, rush patient to the operating room. General anaesthesia, IV antibiotic prophylaxis given and catherised. Abdomen entered through a transverse suprapubic inscision.
The affected tube is brought out and salpingectomy is performed. Strict haemostatsis secured. Peritoneal cavity cleared of blood and blood products. Mops and instruments counted and abdomen closed in layers.
Blood transfused depending on the amount of loss and post op hemoglobin.
Inj Anti D immunoglobulin given if the lady is Rh negative and husband
Rh positive
Patient should be advised to report immediately in future pregnancies
d) Referral Criteria:
When an unruptured ectopic pregnancy is diagnosed and facilities are lacking for timely monitoring of serum beta hcg titres and medical management. When patient is stable and facilities or skill to offer laparoscopic surgery are not available.
When heterotopic pregnancy is diagnosed and patient is desirous of continuing with the intrauterine conception.
After a life saving laparotomy, for need of blood transfusion.
Situation 2: At Superspeciality Facility in Metro location where higher end technology is available.
a) Clinical diagnosis: Similar to situation 1
b) Investigations: As in situation 1.
Special investigations:
1. Serum Beta hCG titres need estimation serially to facilitate expectant management or medical manangement with Methotrexate. When Methotrexate is used:
1. Complete blood count
2. Liver function test
3. Renal function test
c) Treatment:
When ruptured ectopic is diagnosed laparotomy may be done as in situation 1.
When laparoscopy is chosen- Salpingostomy or salpingectomy is peformed.
Expectant management : Proportion of all ectopics will not progress to tubal rupture, but will regress spontaneously and be slowly absorbed. Level of hCG must fall and the woman becomes clinically well.
it is an option for clinically stable asymptomatic women with an ultrasound diagnosis of ectopic pregnancy and a decreasing serum hCG, initially less than serum 1000 iu/l.(ref rcog greentop)
Women managed expectantly should be followed twice weekly with serial hCG measurements and weekly by transvaginal examinations to ensure a rapidly decreasing hCG level (ideally less than 50% of its initial level within seven days) and a reduction in the size of adnexal mass by seven days. Thereafter, weekly hCG and transvaginal ultrasound examinations are advised until serum hCG levels are less than 20 iu/l .
On hcg monitoring if the level increases or plateaues ,active medical management is resorted to.
Medical management with Methotrexate
The most widely used medical treatment at present is intramuscular methotrexate given as a single dose calculated from patient body surface area.
Dose:
A single dose of 1mg/kg body weight or 50mg/square metre body surface area of methotrexate given intramuscularly in addition to leukovorum (folic acid antagonist) 0.1mg/kg IM.
Methotrexate should not exceed 4 doses.
There is 70-95% efficiency in the treated cases.
It takes 4-6 weeks for the complete resolution of ectopic pregnancy with methotrexate.
Methotrexate is also useful in the management of persistent ectopic which is a complication of conservative surgical treatment and incomplete removal of trophoblastic tissue.
Serum hCG levels are checked on days four and seven and a further dose is given if hCG levels have failed to fall by more than 15% between day four and day seven. Large uncontrolled studies have reported that about 14% of women will require more than one dose of methotrexate and less than 10% of women treated with this regimen will require surgical intervention.
Can be considered for women with confirmed or high suspicion for ectopic pregnancy who are hemodynamically stable with no evidence of rupture.
Absolute contraindications are breast feeding, immunodeficiency, alcoholism, blood dyscrasias, active pulmonary disease ,peptic ulcer disease,hepatic renal or hematologic disorder. Gestation sac larger than 3.5 cm and embryonic cardiac motion are relative contraindications.
Medical management with Methotrexated.
Referral criteria:
1. Patients with comorbidities requiring multidisciplinary input.
2. When skilled manpower and facilities are not available.
3. When it is a heterotopic pregnancy usually a consequence of assisted reproductive techniques, referral to an ART center for further care is necessary.
V. Further reading and references:
RCOG guidelines
Williams Obstetrics
Te Linde’s operative gynecology
Novaks text book for gynecology
VI. Resources required for one patient/procedure
| Situation | Human resources | Investigations | Drugs and consumables | Boyles OT Laparotomy set |
| 1. | Gynecologist Anesthetist Nurses 2 | Blood tests | Boyles OT Laparotomy set | |
| 2. | Gynecologist Assistant doctor Anaesthetist Nurses x 3 Sonologist Technicians x2 House keeping Blood bank officer | Blood tests HCG quantitative | Methotrexate | Boyles OT Laparotomy set Laproscopy set Laboratory Ultrasound machine |

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd