- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
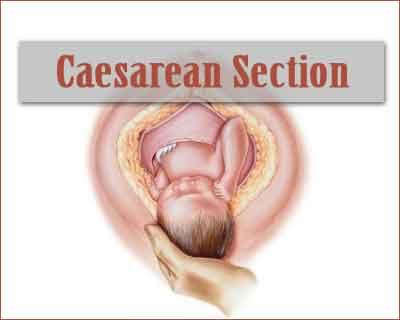
Standard Treatment Guidelines For Caesarean Section
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Caesarean Section. Following are the major recommendations :
I. Incidence in our country:
10 to 50% depending on the level of care- whether a primary or tertiary referral center.
Clinical Diagnosis:
Common indications recognizable during the antenatal period that may require cesarean section are malpresentations, antepartum haemorrhage, previous caesarean section or surgery on the uterus, bad obstetric history, IUGR, induction of labour for pre eclampsia, gestational diabetes, postdatism, premature rupture of membranes, fetal macrosomia, and cephalopelvic disproportion.
Intrapartum indications include fetal distress, dysfunctional/ prolonged labour, malpresentations, obstructed labour and cord prolapse.
Pre-operative Investigations:
Hb%, BT, CT, urine routine, blood grouping, cross matching and reservation of blood
Ultrasound for presentation, placental position, biophysical profile.
Timing of Caesarean Section:
Elective LSCS should be done preferably after 39 weeks to decrease neonatal morbidity.
Emergency LSCS should be done within 30 minutes of decision if there is immediate threat to life of women or foetus.
Emergency cesarean may be done up to 75 minutes when there is maternal or foetal compromise which is not life threatening.
Treatment: IV line and Oxygen inhalation, Regional or general anaesthesia
Pre-operative:
Informed Consent
Prepare abdomen, perineum and back
IV line to be established and bladder catherisation
Parenteral H2 blocker and antiemetic
IV antibiotic to be given before skin incision (Avoid co-amoxyclav)
Operative details:
Abdominal incision could be transverse suprapubic or vertical.
The uterine incision is usually transverse in the lower segment, midline vertical (Classical) may be indicated occasionally if lower segment is unapproachable due to dense adhesions.
Baby is extracted, cord clamped, cut and baby handed over to the paediatrician. Cord blood should be collected in Rh isoimmuniation cases. Placenta with entire membranes removed by controlled cord traction. Oxytocics administered to contract the uterus and prevent post patum haemorrhage. Uterus sutured with absorbable sutures to secure haemostasis in two layers. No need of suturing the peritoneum. Uterus should not be exteriorised routinely. Surgical mops and instrument count to be checked. Abdominal wall closed in layers.
Post operative:
Vitals, urine output, and bleeding are monitored,
IV fluids, antibiotics and pain medication given,
DVT prophylaxis advised if indicated,
Oral feeds encouraged with return of bowel sounds after 8 hours.
Early breast feeding and ambulation encouraged.
Situation 1: At Secondary Hospital/ Non-metro situation: Optimal Standards of treatment in situations where technology and resources are limited.
Cases warranting immediate delivery to save the life of baby or mother should be dealt with. In situations where skilled manpower and technology is not available, woman may to be referred to higher institution.
Situation 2: At super-specialty facility in metro location where higher end technology is available.
Referral criteria: Situations warranting neonatal intensive care management facilities, need for blood and blood component therapy, special anaesthesia services like epidural analgesia; For the management of post operative complications of caesarean section like sepsis, secondary haemorhage, wound dehiscence, acute renal failure etc where multidisciplinary input is warranted need to be tackled at super-specialty level.
Additional Investigations that may be required:
Ultrasound Doppler studies in IUGR
Electronic fetal monitoring in labour
TSH, LFT, RFT, Coagulation profile tailored to the needs of the patient.
Further Reading/ References:
RCOG Guidelines
Williams text book of Obstetrics
Resources required for one patient/procedure
| Situation | Human resources | Investigations | Drugs and consumables | Equipment |
| 1. | Obstetrician Anaesthetist Nurse Floor nurse House keeping | Written above | parenteral H2 blocker antiemetic IV antibiotic oxytocin | Boyles OT table with lateral tilt of 15 degree or wedge Light Section tray Suction apparatus Baby Warmer electrocautery |
| 2. | Senior obstetrician Junior doctor Consultant Anesthetist Nurses x2 floor Nurse OT technician Senior Hematologist Experienced pediatrician | Other Drugs as per individual patient | Boyles Ot table Light Section tray Suction apparatus Baby Warmer Electrocautery Critical care bed |

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd