- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Spine Injury - Standard Treatment Guidelines

With an estimated annual incidence of 300 per crore population, approximately 40,000 new spine injury cases are added every year in India. 40% of these are complete lesions i.e. tetra or paraplegia. The socio economic impact of spinal injuries is huge with 85% of victims being male in the age group of 15 to 35 years. Management of patients who have sustained spinal cord injury requires careful assessment and management. Inadequate assessment and management of these injuries may lead to worsening of existing spinal cord injury or the production of a new cord injury.
The Ministry of Health and Family Welfare has issued the Standard Treatment Guidelines Orthopaedics Guidelines for spine injury. Following are the major recommendations:
Case definition:
For both situations of care (mentioned below*)
Spinal cord injury (SCI) is an insult to the spinal cord resulting in a change, either temporary or permanent, in its normal motor, sensory, or autonomic function.
Incidence of The Condition In Our Country :
In the absence of a national spinal cord injury registry in India, the exact incidence is not known. Approximately 30 cases per million population. Approximately 40% of these will be complete. Majority of the cases are due to road side accidents or fall from height.
Differential Diagnosis :
All trauma patients should be assumed to have a spinal injury and treated as such till a detailed clinical examination and radiological investigations has been performed. Potential spinal cord injury should be suspected in following situations:
a. Altered mental status.
b. Evidence of intoxication.
c. Associated head injury, extremity fracture
d. Focal neurological deficit.
e. Spinal pain or tenderness
f. Mechanism of injury e.g fall from height, fall on head, whiplash injuries, high energy injuries
Prevention And Counseling :
All trauma patients should be assumed to have a spinal injury and treated as such, until this can be confidently excluded. Full spinal immobilisation should be employed including a collar, spinal board and blocks. Tape can be used to secure the head to the blocks. This should be done as soon as physically possible and prior to moving the patient to a site of definitive care.
Optimal Diagnostic Criteria, Investigations, Treatment & Referral Criteria
*Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited
Clinical Diagnosis:
After the ABC have been taken care of, the patient is gently log rolled and whole of the spine is palpated for tenderness or a palpable step-off deformity. Neurogenic shock, incontinence of bowel, bladder and penile erection indicate severe spine injury. A careful and detailed neurological examination is then performed and meticulously documented.
Assessment of motor function:
| Diaphragm | C3-5 |
| Shrug shoulders | C4 |
| Deltoids/elbow flexion | C5 |
| Extend wrist | C6 |
| Extension of elbow/ flexion of wrist | C7 |
| Abduct fingers | C8 |
| Active chest expansion | T1-T12 |
| Hip flexion | L2 |
| Knee extension | L3-4 |
| Ankle dorsiflexion Ankle plantar flexion | L5-S1 S1-2 |
Assessment of sensory function
| Deltoid area | C5 |
| Thumb | C6 |
| Middle finger | C7 |
| Little finger | C8 |
| Nipple | T4 |
| Xiphoid | T8 |
| Umblicus | T10 |
| Symphysis | T12 |
| Anterior thigh | L2 |
| Anterior knee | L3 |
| Antero-lateral ankle | L4 |
| Dorsum of great and 2nd toe | L5 |
| Lateral side of foot | S1 |
| posterior calf | S2 |
| perianal sensation | S2-5 |
Frankel’s grades : Spinal Cord Injury is most commonly graded using Frankel’s grades (A to E).
A; Complete motor and sensory loss
B: Sensation only present below lesion
C: Sensations present and motor function is present but useless
D: Motor useful but not normal
E: No neurological deficit.
After the motor and sensory examination, presence of sacral sparing may be noted by voluntary rectal sphincter tone and toe flexor contractions. Presence of sacral sparing indicates a better neurological prognosis.
Although spinal shock is over by 24 hours, rarely it may be prolonged. A positive bulbocavernous reflex or a positive anal wink indicates the end of spinal shock. If no motor or sensory function can be documented at this stage, a complete spinal cord injury is present.
Investigations:
All patients with suspected spinal injury should have radiographic evaluation.
1. Initial screening can be done by conventional antero-posterior and lateral x-rays. The cervical spine radiographs must include the C7-T1 junction to be considered adequate
2. Additional Open-mouth views should be done to evaluate odontoid injury.
3. Whole spine should be evaluated with a patient of spinal injury.
4. The patient should be referred for advanced diagnostic modalities only when the patient is stable:
CT Scan : CT scan cervical spine in all cases of head injuries or intoxication at the same time as the brain CT. CT should be done when plain X-Ray is inadequate particularly upper cervical spine injuries and C7-T1 junction.
MRI : MRI is essential for evaluating injury to the soft tissues and ligaments, discs, intrinsic cord damage (oedema, hematoma, or contusion) and Para vertebral soft tissues. MRI is particularly useful in scenarios such as central cord syndrome where plain radiographs will not show any fractures or dislocations. If possible MRI should be done before the cervical traction is applied. In patients with preinjury morbidities such as Ankylosing Spondylitis, CT and MRI should be done to rule out occult instability even if x-rays are normal.
Treatment :
Standard Operating procedure
a. In Patient
1. Once the patient with a potential spinal injury reaches the emergency, the patient should be transferred off the backboard onto a firm padded surface while maintaining spinal alignment. A baseline skin assessment can be performed at the time of shifting the patient from spine board to hospital bed.
2. Adequate number of personnel should be employed for logrolling during patient repositioning, turning and transfers.
3. Secure ABC
a. Airway: If intubation is required rapid sequence intubation with manual inline stabilisation should be done. Awake fibreoptic intubation is ideal in a cooperative patient and if facilities are available.
b. Prevent and treat hypotension
i. Look for other causes of hypotension such as abdominal, chest and pelvic injury
ii Look for Neurogenic shock i.e. hypotension with bradycardia in cervical spine and high thoracic injuries.
c. Monitor and regulate temperature
4. Perform a baseline neurological assessment on any patient with suspected spinal injury. Determine a neurological level and the completeness of injury (as described above). Perform serial examinations as indicated to detect neurological deterioration or improvement. The neurological examination should be done as per an objective system such as ASIA scoring system and documented properly. Perform serial examinations as indicated e.g. after each intervention to detect neurological deterioration or improvement.
5. Once initial resuscitation is done, complete a comprehensive tertiary trauma survey in the patient with potential or confirmed spinal cord injury.
6. In the patient with acute spinal cord injury, particularly higher cervical injury, assess and document early and frequently any evidence of traumatic brain injury (TBI) in the form of loss of consciousness and posttraumatic amnesia.
7. Screen for thoracic and intra-abdominal injury in all patients with spinal cord injury.
8. No clinical evidence exists to definitively recommend the use of any neuroprotective pharmacologic agent, including steroids, in the treatment of acute spinal cord injury to improve functional recovery. However high dose methyl-prednislone may be used as per NASCIS III recommendations (Methylprednisolone: Bolus dose of 30 mg/kg of body weight over 15 minutes, followed by a 45-minute pause, and then a 23-hour continuous infusion of 5.4 mg/kg/hr, If patient presents between 3 and 8 h, give the above steroid infusion for total of 48 h) if the patient presents within 8 hours of injury. The risk of complications such as such as higher infection and sepsis rates, respiratory complications and gastrointestinal hemorrhage should be kept in mind while administering steroids.
9. Genitourinary Tract :
- Place an indwelling urinary catheter as part of the initial patient assessment unless contraindicated
- Leave indwelling urinary catheters in place at least until the patient is haemodynamically stable
- CIC should be taught to patient or the relatives as soon as the patient is stable
10. Gastrointestinal Tract
- Initiate stress ulcer prophylaxis
- Evaluate swallowing function prior to oral feeding in any acute SCI patient
11. Measures to prevent bed sores:
- Assess areas at risk for skin breakdown frequently.
- Place the patient on a pressure-reduction mattress or a mattress overlay depending on the patient's condition.
- Use a pressure-reducing cushion when the patient is mobilized out of bed to a sitting position.
- Reposition to provide pressure relief or turn at least every 2 hours while maintaining spinal precautions.
- Keep the area under the patient clean and dry and avoid temperature elevation.
- Assess nutritional status on admission and regularly thereafter.
- Inspect the skin under pressure garments and splints.
- Educate the patient and family on the importance of vigilance and early intervention in maintaining skin integrity.
b. Out Patient care
A secondary hospital is expected to provide outpatient care to the spinal cord injury patients who may be referred back from specialized centers after definitive treatment. This may be in form of
i. physiotherapy for passive mobilisation of all joints and active exercises for muscles
ii. Teaching of clean intermittent cathetrisation
iii. Counselling of the patient and attendants
iv. Care of bed sores
c. Day Care Day
care might be needed for situations like debridement of bed sores.
Referral criteria:
1. The patient should be hemodynamically stable and fully resuscitated at the time of referral
2. All the patients who need surgery (indications discussed in the next section) need to be referred to a specialized tertiary care centre.
3. The decision of need for surgery can only be made by an experienced spinal surgeon either orthopedic or neurosurgeon. In absence of these all patients with proven or suspected spine injury should be referred to a higher center.
4. It is desirable to have a two way communication with higher center while referring a patient.
*Situation 2: At Super Specialty Facility in Metro location where higherend technology is available
Clinical Diagnosis:
After the ABC have been taken care of, the patient is gently log rolled and whole of the spine is palpated for tenderness or a palpable step-off deformity. Neurogenic shock, incontinence of bowel, bladder and penile erection indicate severe spine injury. A careful and detailed neurological examination is then performed and meticulously documented.
Assessment of motor function:
| Diaphragm | C3-5 |
| Shrug shoulders | C4 |
| Deltoids/elbow flexion | C5 |
| Extend wrist | C6 |
| Extension of elbow/ flexion of wrist | C7 |
| Abduct fingers | C8 |
| Active chest expansion | T1-T12 |
| Hip flexion | L2 |
| Knee extension | L3-4 |
| Ankle dorsiflexion Ankle plantar flexion | L5-S1 S1-2 |
Assessment of sensory function
| Deltoid area | C5 |
| Thumb | C6 |
| Middle finger | C7 |
| Little finger | C8 |
| Nipple | T4 |
| Xiphoid | T8 |
| Umblicus | T10 |
| Symphysis | T12 |
| Anterior thigh | L2 |
| Anterior knee | L3 |
| Antero-lateral ankle | L4 |
| Dorsum of great and 2nd toe | L5 |
| Lateral side of foot | S1 |
| posterior calf | S2 |
| perianal sensation | S2-5 |
Frankel’s grades : Spinal Cord Injury is most commonly graded using Frankel’s grades (A to E).
A; Complete motor and sensory loss
B: Sensation only present below lesion
C: Sensations present and motor function is present but useless
D: Motor useful but not normal
E: No neurological deficit.
After the motor and sensory examination, presence of sacral sparing may be noted by voluntary rectal sphincter tone and toe flexor contractions. Presence of sacral sparing indicates a better neurological prognosis.
Although spinal shock is over by 24 hours, rarely it may be prolonged. A positive bulbocavernous reflex or a positive anal wink indicates the end of spinal shock. If no motor or sensory function can be documented at this stage, a complete spinal cord injury is present.
Investigations:
Radiographic evaluation of patients with spinal injury.
1.Initial screening can be done by conventional antero-posterior and lateral xrays.
2. Additional Open-mouth views should be done to evaluate odontoid injury.
3. Special views like swimmer’s view and oblique views can be done to see junctional areas
4. CT scan of the whole spine should be done if in presence of clinical suspicion but fractures cannot be demonstrated on x rays or if junctional areas are not visualised.
5. MRI should be done to evaluate ligamentous injury, spinal cord injury. In patients with pre-injury morbidities such as AS,DISH, stiff spine CT and MRI should be done to rule out occult instability even if x-rays are normal.
6. Whole spine should be evaluated with a patient of spinal injury.
Treatment:
Standard Operating procedure
a. In Patient
1. Once the patient with a potential spinal injury reaches the emergency , the patient should be transferred off the backboard onto a firm padded surface while maintaining spinal alignment. A baseline skin assessment can be performed at the time of shifting the patient from spine board to hospital bed. Adequate number of personnel should be employed for logrolling during patient repositioning, turning and transfers.
2. Secure ABC
a. Airway : If intubation is required rapid sequence intubation with manual inline stabilisation should be done. Awake fibreoptic intubation is ideal in a cooperative patient and if facilities are available.
Prevent and treat hypotension
i. Look for other causes of hypotension such as abdominal, chest and pelvic injury
ii. Look for Neurogenic shock i.e. hypotension with bradycardia in cervical spine and high thoracic injuries.
iii. Monitor and regulate temperature.
3. Perform a baseline neurological assessment on any patient with suspected spinal injury . Determine a neurological level and the completeness of injury. Perform serial examinations as indicated to detect neurological deterioration or improvement. The neurological examination should be done as per an objective system such as ASIA scoring system and documented properly. Perform serial examinations as indicated e.g. after each intervention to detect neurological deterioration or improvement. ASIA score is very elaborate, one can follow TLISS/ TCLISS (as recommended by STSG)
4. No clinical evidence exists to definitively recommend the use of any neuroprotective pharmacologic agent, including steroids, in the treatment of acute spinal cord injury to improve functional recovery. However high dose methyl-prednislone may be used as per NASCIS III recommendations (Methylprednisolone: Bolus dose of 30 mg/kg of body weight over 15 minutes, followed by a 45-minute pause, and then a 23-hour continuous infusion of 5.4 mg/kg/hr, If patient presents between 3 and 8 h, give the above steroid infusion for total of 48 h) if the patient presents within 8 hours of injury. The risk of complications such as such as higher infection and sepsis rates, respiratory complications and gastrointestinal hemorrhage should be kept in mind while administering steroids, It is basically a treatment option,not standard care.
5. Once initial resuscitation is done, complete a comprehensive tertiary trauma survey in the patient with potential or confirmed spinal cord injury.
6. In the patient with acute spinal cord injury, particularly higher cervical injury, assess and document early and frequently any evidence of traumatic brain injury (TBI) in the form of loss of consciousness and posttraumatic amnesia
7. Screen for thoracic and intra-abdominal injury in all patients with spinal cord injury.
8. Perform early stabilization of extraspinal fractures. Perform this surgery as early as possible to facilitate early rehabilitation and concomitantly with any required spinal stabilization if the patient is medically stable.
9. Surgical treatment
a. Perform a closed or open reduction as soon as permissible on patients with bilateral cervical facet dislocation in the setting of an incomplete spinal cord injury
b. Consider early spinal stabilization where indicated
c. Consider early surgical spinal canal decompression direct or indirect in the setting of a deteriorating spinal cord injury as a practice option that may improve neurologic recovery, although there is no compelling evidence that it will.
The following algorithms may be followed as a guide to help in decision making in operative treatment of spine injuries. These algorithms are meant as a guide and the treatment plan for each patient needs to be individualised
i) Upper cervical injuries
a) Occipital condyle fractures
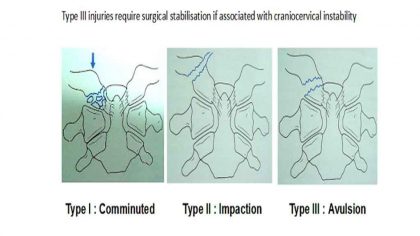
b) Atlas fractures
Surgical stabilisation if:
- neurologic symptoms,
- instability is more than 5 mm on dynamic radiographs
- significant pain is present with the evidence of nonunion.
The surgical procedure is stabilization of C1-C2 or occiput-C2
c) Odontoid factures:
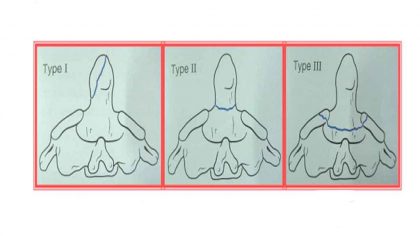
• Anterior screw fixation in type 2 fractures. This is contraindicated in TAL injury,Comminuted fracture,Anterior oblique fractures ,Nonunion>3 months Osteoporosis ,Barrel chest. Posterior arthrodesis can be done in such cases.
d) Hangman fractures: Type 3 require stabilization.
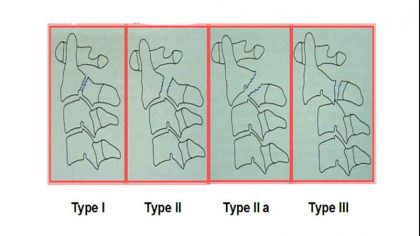
ii) Subaxial Cervical Spine Injuries
10. Adjunctive measures:
- Assess areas at risk for skin breakdown frequently.
- Place the patient on a pressure-reduction mattress or a mattress overlay depending on the patient's condition.
- Use a pressure-reducing cushion when the patient is mobilized out of bed to a sitting position.
- Reposition to provide pressure relief or turn at least every 2 hours while maintaining spinal precautions.
- Keep the area under the patient clean and dry and avoid temperature elevation.
- Assess nutritional status on admission and regularly thereafter.
- Inspect the skin under pressure garments and splints.
- Educate the patient and family on the importance of vigilance and early intervention in maintaining skin integrity.
11. Genitourinary Tract
Place an indwelling urinary catheter as part of the initial patient assessment unless contraindicated
Leave indwelling urinary catheters in place at least until the patient is haemodynamically stable
CIC should be taught to patient or the relatives as soon as the patient is stable
12. Gastrointestinal Tract
- Initiate stress ulcer prophylaxis.
- Evaluate swallowing function prior to oral feeding in any acute SCI patient with cervical spinal cord injury, halo fixation, cervical spine surgery, prolonged intubation, tracheostomy
b. Out Patient
Out patient care is needed for non surgically treated patients on ambulatory care andSurgically treated patients. This will entail:
Prescription of appropriate orthoses
Physiotherapy services
Counselling: social, psychological,vocational
Referral criteria:
Surgically treated patients may be referred back to secondary hospitals for physiotherapy, and care of back, bladder and bowel.
WHO DOES WHAT? and TIMELINES
a. Doctor
Primary assessment and resuscitation
Clinical diagonosis
Ordering and interpretation of investigations
Clinical decision making
Surgical procedures
b. Nurse
Primary resuscitation can be performed by a nurse
Prevention of bed sores
Maintenance of inventory(drugs,consumables etc.)
Operating room assistance
c. Technician
Pre trauma technicians do primary immobilization and do safe transport to hospitals
Primary resuscitation can be performed by technicians
Appropriate radiological investigations
Physiotherapy
Guidelines by The Ministry of Health and Family Welfare :
Dr. P.K. DAVE, Rockland Hospital, New Delhi
Dr. P.S. Maini, Fortis Jessa Ram Hospital, New Delhi
Reviewed By
Dr. V.K. SHARMA Professor Central Instiute of Orthopaedics Safdarjung Hospital New Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd