- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Small increases in complications when knee replacement done as outpatient procedure
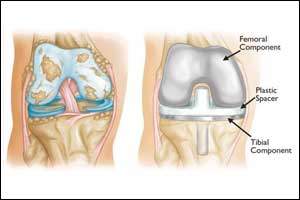
Some complications are more common when total knee replacement surgery is done as an outpatient or same-day procedure, reports a study in the December 2017, issue of The Journal of Bone & Joint Surgery. The journal is published in partnership with Wolters Kluwer.
Compared to conventional inpatient surgery, patients undergoing outpatient total knee arthroplasty (TKA) experience higher rates of certain complications, including infections, repeat surgery, and blood clots, according to the new research by Armin Arshi, MD, of the David Geffen School of Medicine at UCLA and colleagues.
As Inpatient TKA Becomes More Common, Concern about Increased Complications
Using a US insurance database, the researchers identified two groups of patients who had a TKA procedure between 2007 and 2015. About 4,400 patients underwent TKA on an outpatient basis, generally sent home on the same day as surgery. Another 129,000 patients underwent conventional inpatient TKA, typically staying in the hospital for one or more days after surgery.
Dr. Arshi and colleagues compared rates of various complications over 1 year between the two groups. The patients in both groups had a median age between 70 and 74 years, but based on a standard "comorbidity" score, the outpatient TKA group had fewer accompanying medical problems.
The results showed that several joint-related and medical complications were more frequent after outpatient TKA. The most common complication--knee pain and stiffness requiring joint manipulation with the patient under anesthesia--occurred in 4.24 percent of patients undergoing outpatient TKA versus 3.57 percent of the inpatient TKA group. After adjustment for age, sex, and comorbidity, outpatient TKA patients had a relative 28 percent increase in the risk of this complication.
Outpatient TKA was also associated with relative increases of 50 percent in surgical infections requiring irrigation and debridement, 22 percent in repeat surgery due to causes other than infection, and 35 percent in the removal of the knee prosthesis. (Absolute rates of these complications were low. For example, implant removal at 1 year occurred in 0.50 percent of outpatient TKAs versus 0.44 percent of inpatient TKAs.)
Two medical complications were also more frequent in the outpatient TKA group. The 60-day risk of deep vein thrombosis, a blood clot-related complication, was 42 percent higher, relative to inpatient TKA. There was also a small but significant 13 percent increase in the 14-day risk of acute kidney failure.
There is growing interest in performing TKA as an outpatient procedure to avoid the costs associated with hospitalization for this common procedure. While some studies have reported good outcomes, there are still limited data on the safety and effectiveness of outpatient TKA, which remains relatively uncommon.
The new analysis suggests that some complications are more common after outpatient TKA, compared to conventional inpatient TKA. The findings are concerning because the number of knee replacements is expected to increase severalfold over the next 20 years and because patients selected for outpatient TKA are typically healthier and have better functional status--and thus should be at lower risk of complications.
The findings point to some important "clinical pathways for realizing the potential for safe and effective outpatient arthroplasty," the researchers believe.
"The findings are particularly important to patients who may want to ask their surgeon whether or not they are medically optimal candidates for outpatient surgery and whether they will receive the standard antibiotic and thromboembolism prophylaxis protocols postoperatively," Dr. Arshi comments. "We also recommend that they consider plans for physical therapy and rehabilitation after discharge, and in particular whether they will have adequate access to important rehabilitation at home during the important early postoperative period."
Senior author Nelson F. SooHoo, MD, comments: "Given the low absolute rates of complications in both groups, it is likely that outpatient TKA will emerge as a safe option in the setting of postoperative care pathways that ensure equivalent attention to rehabilitation, antibiotic, and thromboprophylaxis as current inpatient protocols."

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd