- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Ruptured Abdominal Aortic Aneurysm Misdiagnosed as Acute Appendicitis
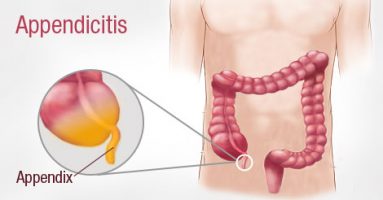
A ruptured abdominal aortic aneurysm is a serious life-threatening condition, which is usually prevalent in old age group. Unusual presentation in a young patient is very difficult to diagnose and necessitates high index of suspicion. Any deviation from the normal presentation of acute appendicitis mandates further investigation.
This case report presents a very rare cause of abdominal pain in a young patient that mimic acute appendicitis. The patient had abdominal CT scan, which revealed extensive abdominal aortic aneurysm with impending rupture. He was immediately transferred to tertiary hospital to be evaluated and managed by the vascular surgeon. Emergent surgery was performed with uneventful recovery.
Acute appendicitis is the most common cause of abdominal pain in the young patient. However, treating surgeon should have a high index of suspicious for any other causes the mimic acute appendicitis and could carry very high morbidity and mortality if not diagnosed early.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd