- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Role of 3-D Printing in surgical management of cardiovascular diseases- Dr Harinder Singh Bedi
Three-dimensional (3D) printing is a fabrication technique used to transform digital objects into physical models. The technique builds structures of arbitrary geometry by depositing material in successive layers on the basis of a specific digital design. Although the use of 3D printing technology in cardiovascular medicine is still a relatively new development, advances within this discipline are occurring at a rapid rate.
Three-dimensional (3D) printing is at the crossroads of printer and materials engineering, noninvasive diagnostic imaging, computer-aided design, and structural heart intervention. Cardiovascular applications of this technology include the use of patient-specific 3D models for medical teaching, exploration of valve and vessel function, surgical and catheter-based procedural planning, designing and refining the latest innovations in percutaneous structural devices and in creating functional organs and finally printing a tailor-made genetically patient specific working heart.
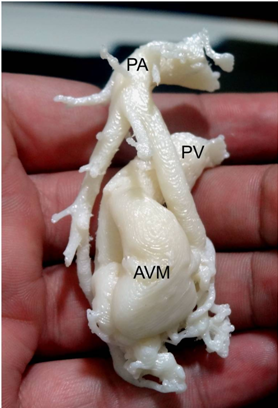
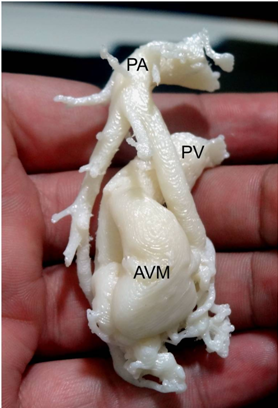 The 3 D printed model of the pulmonary AVM
The 3 D printed model of the pulmonary AVMCardiovascular Applications
3D-printed patient-specific models can be created for a number of different applications including creation of anatomic teaching tools, development of functional models to investigate intracardiac flow, creation of deformable blended-material models for complex procedural planning and to create or refine intra-cardiac devices. A heart patch capable of contracting has obvious applications in replacing parts of scarred infracted heart tissue. A synthetic 3D printed heart which can pump blood is being investigated. The ultimate goal is to print a functioning artificial heart using the patient’s own cells so that there is no immune rejection.
We have used this technology in a case of a large complex AV Malformation (AVM) of the lung (the first time in the world that this has been done ), printing of custom made ribs in a case of cancer of the rib cage , and in a case of mitral valve regurgitation needing a repair to help us with understanding the disease , planning the various options, counseling the patient, teaching younger colleagues and performing a flawless surgery . The AVM case (figure 1) was published in CTS Net 1.
CARDIOVASCULAR APPLICATIONS :
- Teaching tools
Like the familiar plastic heart models, a 3D-printed model can rapidly convey a complex anatomic arrangement, with the added value of also depicting patient-specific anatomic pathology. Patient-specific models of congenital heart defects have been used for critical-care training of residents and nurses, and have shown the potential to enhance the communication between surgeons and patients. The model can be made to be opened up to see the inner structures eg complex multiple ventricular septal defects. In these times of paucity of cadavers – a printed organ can be easily used for teaching purposes. It can be replicated multiple times at a very low cost.
- Functional flow models
3D patient-specific models of diseased valves, congenital defects, and coronary arteries can be readily created by combining the technologies of high-spatial-resolution CT, CAD software, and multi-material 3D printing. Such models may be especially useful for evaluating clinically challenging situations, such as the noninvasive quantification of paravalvular regurgitation severity under controlled flow conditions or for the planned deployment of endovascular stents. These models also have the potential to simulate devices such as plugs for defects or new coronary stents which can be readily evaluated within this patient-specific coronary bed.
- Procedural planning
Congenital cardiovascular diseases are often associated with complex and unique geometry that can be very difficult to fully appreciate from 2D CT, CMR, or echocardiographic images as in our case of complex pulmonary AVM. As such, 3D-printed modeling may play a key role to provide a more comprehensive understanding and functional evaluation of various congenital heart conditions. These models have recently been used to plan first-in-man structural heart procedures to repair MV function deploying both a MitraClip device as well as an occluder device to treat severe MV regurgitation 2. True to life 3D models prevent mistakes and promote innovation in the treatment of specific structural heart interventions.
- Device innovation
The ability to test new or revised structural heart repair devices within a range of cardiac pathologies is particularly appealing. Although other modeling options have been relied upon for many years, device development using cadaveric models cannot be used for specific-patient procedure planning. Likewise, animal models invariably lack either the correct size or the pathological element (e.g., calcification) of human cardiovascular conditions.
- Functional organs:
At the turn of this decade, several research teams have produced organs on a chip, that is devices that can model the working (from a chemical point of view) of a human organ, like a liver or a kidney.
Very recently a group in Israel has managed to print a tiny heart with vessels – the cells used were human ones 3. This is the first step of a long way to produce a custom made fully functional complete heart which may finally overcome the problem of paucity of donors.
The obvious advantages of the presently available 3D printing technology that we have used in 3 cases are : it makes planning of a complex lesion so much more precise, one can plan options (A, B, etc), it avoids emergency planning in OT, leads to a better counseling of patient and relatives, is good for training – a clinical transfer tool – it is like a batting practise, it allows the surgeon to see around corners – a prescient pre-visualisation , it allows the surgeon to ‘see’ through blood, it gives a trial run, leads to reduced OT time, reduced CPB time , there is a reduced chance of a residual lesion, less chances for re-intervention, is better for training , one can assess hemodynamics by putting in a virtual valve , close a defect etc, and it is invaluable for planning a refined approach by a pre-procedural planning
Future Directions
By combining the technologies of high-spatial-resolution cardiac imaging, image processing software, and fused dual-material 3D printing, several hospital centers have recently demonstrated that patient-specific models of various cardiovascular pathologies may offer an important additional perspective on the condition. Patient-specific 3D MV models may directly affect our ability to select appropriate patients for structural heart therapy and anticipate procedural complications, and may potentially revise and improve the flood of intracardiac devices that are rapidly becoming available for therapeutic use. Within a limited range of physiological performance, the native cardiac elements (e.g., vessel wall, chamber wall, and valve leaflet) can be modeled from a wide spectrum of 3D print material blends. This notion of a personalized 3D-printed cardiovascular prosthesis is not here today but is now clearly visible on the horizon. The ultimate holy grail is the fully functional heart made from the patient’s own cells.
With applications in congenital heart disease, coronary artery disease, and surgical and catheter-based structural disease, 3D printing is a new tool that is challenging how we image, plan, and carry out cardiovascular interventions.
References :
- https://www.ctsnet.org/article/three-dimensional-printing-guided-precise-surgery-complex-pulmonary-arteriovenous
- Little SH, Vukicevic M, Avenatti E, Ramchandani M , Barker CM . 3D Printed Modeling for Patient-Specific Mitral Valve Intervention Repair With a Clip and a Plug. JACC 2016, 9: 973-5
- Noor N, Shapira A, Edri R, Gal I, Wertheim L, Dvir T. 3D Printing of Personalized Thick and Perfusable Cardiac Patches and Hearts . Advanced Science 2019 . DOI: 10.1002/advs.201900344
Dr Harinder Singh Bedi is a Senior Consultant Cardio Vascular Endovascular & Thoracic Surgeon in Punjab

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd