- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Risky to attempt SAVR within 3 months of a stroke : Study
The previous stroke is a major risk factor for recurrent ischemic stroke and major adverse cardiac event (MACE) in patients undergoing surgical aortic valve replacement (SAVR), especially if the time elapsed between previous stroke and surgery is less than 3 months, suggests a study published in the journal JAMA Cardiology.
The study was conducted by Charlotte Andreasen, Copenhagen University Hospital, Hellerup, Denmark, and colleagues, with an objective to evaluate the association of time elapsed between previous stroke and SAVR with the risk of recurrent perioperative stroke, MACE, and mortality among patients with aortic valve stenosis.
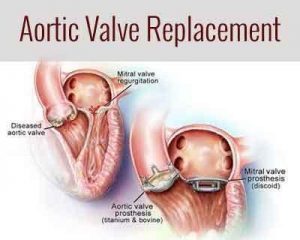
SAVR is a surgery done for replacement of an aortic valve in conditions of aortic valve stenosis and aortic valve regurgitation. During this surgery, the damaged valve is removed and replaced with an artificial valve. The valve replacement is typically an open-heart surgery.
Progression of aortic valve stenosis is medically unpreventable. Likewise, the mortality rate among severely symptomatic patients is markedly increased unless aortic valve replacement is performed. Ischemic stroke is a feared complication of SAVR and prior stroke is a well-established risk factor for periprocedural stroke. Recurrent stroke is associated with more severe functional disability, greater financial burden, and increased mortality compared with an incident stroke. Consequently, it is of particular relevance to investigate the association of time elapsed between previous stroke and SAVR with the risk of adverse outcomes in patients with aortic valve stenosis.
For carrying out the cohort study, the researchers used data from Danish administrative registries and included all patients with aortic valve stenosis older than 18 years who underwent SAVR between 1996 and 2014 (n = 14 030). Patients who received simultaneous mitral, tricuspid, or pulmonary valve surgery and patients with endocarditis 1 year prior to surgery were excluded.
Based on the study, the researchers found out that the rate of SAVR-related ischemic stroke was about 18% in that early period after a prior stroke, compared with 1.2% for patients without prior stroke. This corresponded to a 14-fold jump in adjusted risk. That compared to only a 2-fold to 4-fold risk increase for SAVR performed later than 3 months after a stroke, reported investigators in Denmark based on their nationwide 14,000-patient cohort study. The risk for major adverse cardiac events (MACE: acute MI, ischemic stroke, or cardiovascular death) related to SAVR, meaning within 30 days of the procedure, followed a similar time pattern.
"Therefore, the data suggest that the increased risk of MACE was mainly driven by the increased risk of stroke," Dr. Andreasen told theheart.org | Medscape Cardiology.
The findings suggest that any SAVR that is needed after a stroke be delayed for at least 3 or 4 months if possible, to reduce the risk of recurrent stroke.
Delaying it longer could potentially lower the risk even further, but importantly, "the mortality rate among severely symptomatic patients is known to be markedly increased unless aortic valve replacement is performed, and for critically ill patients, postponement may not be an option," said Andreasen.
For further information click on the link: 10.1001/jamacardio.2018.0899

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd