- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Removal of uterus increases risk of osteoporosis
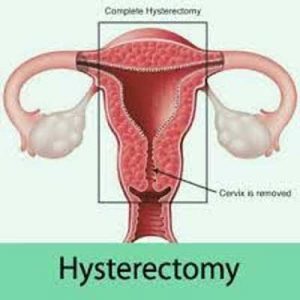
KOREA: Surgical removal of the uterus or hysterectomy before menopause may increase the risk of osteoporosis -- disease in which bones become thinner and more porous from loss of mineral content, according to a recent study published in the American Journal of Obstetrics and Gynecology. This risk is independent of the status of bilateral oophorectomy -- surgical removal of an ovary or ovaries.
Women who undergo hysterectomy experience greater gradual bone mineral loss than women with intact uterus increasing the risk of osteoporosis. "This is because premenopausal hysterectomy decreases follicular atresia, ovarian reserve, and subsequently reduced long-term estrogen secretion," explain the study authors.
Hyo Geun Choi, Hallym University College of Medicine, Anyang, Republic of Korea, and colleagues conducted the study to evaluate the association between hysterectomy without/with bilateral oophorectomy and the occurrence of osteoporosis in premenopausal women.
For the purpose, the researchers extracted data for patients who had undergone hysterectomy (n=9082) and for a 1:4 matched control group (n=36,328) using national cohort study from the Korean National Health Insurance Service. They then analyzed the occurrence of osteoporosis in the two groups. The patients were matched according to age, sex, income, the region of residence, and medical history. Subgroup analyses were performed based on age and bilateral oophorectomy status. The age of the participants was defined as the age at the time of hysterectomy.
Also Read: People with osteoporosis should avoid certain spinal poses in yoga, Mayo Clinic study says
Key Findings:
- The adjusted hazard ratio for osteoporosis was 1.45 in the hysterectomy group.
- The adjusted hazard ratios for osteoporosis in the different age subgroups of this group were 1.84 for ages 40–44 years, 1.52 for ages 45–49 years, 1.44 for ages 50–54 years, 1.61 for ages 55–59 years, and 1.08 for ages ≥60 years.
- The adjusted hazard ratios for osteoporosis according to hysterectomy/oophorectomy status were 1.43 in the hysterectomy without bilateral oophorectomy group and 1.57 in the hysterectomy with bilateral oophorectomy group.
Also Read: Pharmacologic treatment of osteoporosis in postmenopausal women: Endocrine Society guidelines

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd