- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Rare case of Thrombotic Thrombocytopenic Purpura: Case report
Dr Shruti Bhandari and Dr Rohit Kumar, at University of Louisville, Louisville, KY have reported a Classical case of Thrombotic Thrombocytopenic Purpura that has appeared in the New England Journal of Medicine.
Thrombotic thrombocytopenic purpura (TTP) is a rare blood disorder. In TTP, blood clots form in small blood vessels throughout the body. The clots can limit or block the flow of oxygen-rich blood to the body's organs, such as the brain, kidneys, and heart. As a result, serious health problems can develop. The increased clotting that occurs in TTP also uses up platelets (PLATE-lets) in the blood. Platelets are blood cell fragments that help form blood clots. These cell fragments stick together to seal small cuts and breaks on blood vessel walls and stop bleeding.
With fewer platelets available in the blood, bleeding problems can occur. People who have TTP may bleed inside their bodies, underneath the skin, or from the surface of the skin. When cut or injured, they also may bleed longer than normal.
A 35-year-old man presented to the emergency department with a 2-day history of abdominal pain, headache, and brown urine. On examination, his temperature was 37.5°C. He was alert and oriented to time, place, and self, and he had no purpura or petechiae. Laboratory evaluation revealed a hemoglobin level of 8.6 g per deciliter (normal range, 13.7 to 17.5) and a platelet count of 6000 per cubic millimeter (normal range, 140,000 to 370,000).
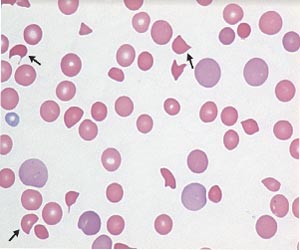
Levels of indirect bilirubin and lactate dehydrogenase were elevated, haptoglobin was undetectable, and the serum creatinine level was 1 mg per deciliter (88 μmol per liter; normal range, 0.6 to 1.3 mg per deciliter [57 to 115 μmol per liter]). Test results for infection with the human immunodeficiency virus were negative. A peripheral blood smear showed numerous schistocytes (arrows). These findings were consistent with microangiopathic hemolytic anemia.
Plasma exchange for suspected thrombotic thrombocytopenic purpura was started immediately. Without the prompt initiation of treatment, mortality from thrombotic thrombocytopenic purpura is high. The patient underwent plasma exchange and received intravenous methylprednisolone for 5 days and had resolution of symptoms and an increased platelet count. The diagnosis was confirmed 2 days after initiation of treatment, with ADAMTS13 activity of 1%. He was discharged with instructions for tapering glucocorticoid treatment. Three months after discharge, he remained well.
For more details click on the link: DOI: 10.1056/NEJMicm1813768

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd