- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Radial-Artery grafts lead to improved outcomes of CABG
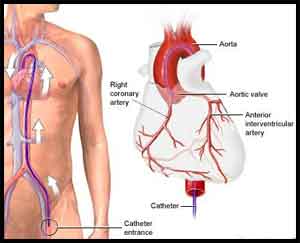
The use of radial-artery grafts for multivessel coronary artery bypass grafting (CABG) improved post-operative outcomes as compared to saphenous-vein grafts, according to a new study published in New England Journal of Medicine.
The study was conducted by John Puskas, MD, of Icahn School of Medicine at Mount Sinai in New York City, and colleagues wherein they performed a patient-level combined analysis of randomized, controlled trials to compare radial-artery grafts and saphenous-vein grafts for CABG.
For carrying out the study, the researchers performed Radial Artery Database International Alliance (RADIAL) meta-analysis of patient-level trial data. Six trials were identified. The primary outcome was a composite of death, myocardial infarction, or repeat revascularization. The secondary outcome was graft patency on follow-up angiography. Mixed-effects Cox regression models were used to estimate the treatment effect on the outcomes.
RADIAL looked at outcomes from 1,036 patients across six trials (534 received radial-artery grafts and 502 received saphenous-vein grafts).
On the basis of the trials, following inferences were made:
- the incidence of adverse cardiac events was significantly lower in association with radial-artery grafts than with saphenous-vein grafts
- the use of radial-artery grafts was associated with a significantly lower risk of occlusion
- the composite outcome of death, myocardial infarction or repeat revascularization was reduced by the multi-artery strategy instead of vein conduit
- the use of radial-artery grafts was associated with a nominally lower incidence of myocardial infarction and repeat revascularization, as compared with the use of the saphenous vein graft
- Death from any cause numerically went in the same direction but with a wide confidence interval (15 versus 17 per 1,000 patient-years, HR 0.90, P=0.68), Mario Gaudino, MD, of New York-Presbyterian and Weill Cornell Medicine in New York City, reported at the American Association for Thoracic Surgery (AATS) meeting in San Diego.
The findings "should guide a genuine change" in how CABG is done, argued Dr. Puskas. "Surgeons in North America and Europe presently use the radial artery in less than 8% of all coronary bypass procedures."
Puskas called RADIAL a landmark study -- and not only for being the first late-breaking study in AATS's more than 100-year history.
"While retrospective observational studies have suggested that this [benefit of radial conduit] might be the case, several randomized controlled trials of radial artery versus saphenous vein grafts as the second conduit in coronary bypass operations have failed to prove a statistically significant improvement in clinical outcomes with the radial artery, because these individual trials have had too few patients enrolled to reach statistical significance," he told MedPage Today.
The authors concluded that as compared with the use of saphenous-vein grafts, the use of radial-artery grafts for CABG resulted in a lower rate of adverse cardiac events and a higher rate of patency at 5 years of follow-up.
For further information, click on the link: 10.1056/NEJMoa1716026

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd