- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Prolonged vasopressor support during hip-fracture surgery increases mortality risk
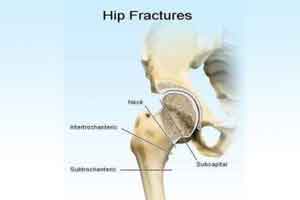
Hip fracture patients treated with vasopressors (VP) infusion ≥3 hours have increased mortality, while patients treated with injections or infusion <3 hours have not, reports a new study published in the journal Acta Anaesthesiologica Scandinavica.
Hip fracture is a common injury in the elderly population and is associated with high morbidity and mortality. Intraoperative hypotension is commonly observed and is often treated with vasopressors (VP).
Johan Kristansson and his associates conducted a study to examine retrospectively how many hip fracture‐patients received VP perioperatively and further to investigate if VP treatment is connected to increased mortality.
Read Also: Hip fractures in the elderly lead to increased all‐cause mortality
The researchers collected data on VP treatment from medical and anaesthesia journals and investigated to find potential confounders. Patients were divided into four groups (a) no VP, (b) VP by injection, (c) VP by infusion <3 hours, and (d) VP by infusion ≥3 hours to achieve stratification. The study included nine hundred and ninety‐seven patients. About 80.4% received VP treatment.
Key study findings:
- The 30‐day mortality rates in subgroups were 3.6%, 5.4%, 6.4% and 19.1% respectively.
- The 90‐day mortality rates were 6.7%, 10.3%, 11.6% and 30.3% respectively. Finally, the same patient groups had 365‐day mortality rates of 12.8%, 20.0%, 23.3% and 44.9% respectively.
- A significant increase was found in mortality (30‐90‐365 days) in patients receiving VP infusion ≥3 hours, after adjusting for confounding factors.
- There was no increased mortality in patients treated by injection and by infusion <3 hours after adjustment for confounding factors vs untreated patients.
For reference log on to https://doi.org/10.1111/aas.13215

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd