- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
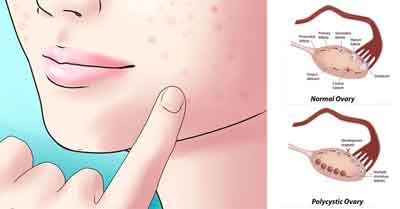
Polycystic Ovarian Syndrome - Standard Treatment Guidelines
Introduction
Polycystic Ovarian Syndrome (PCOS) is the commonest endocrine disorder of the reproductive age group females. Though the structural term “polycystic” is an integral part of its name, the presence of polycystic ovaries is not an essential component of the condition. In fact, PCOS is a functional disorder of the ovaries characterised by complete or incomplete triad of chronic oligo-/anovulation, hyperandrogenism and, sonologically detectable “polycystic” ovaries.
PCOS is known to have significant association with some very important medical conditions like metabolic syndrome, diabetes, cardiovascular disease, endometrial cancer and, obstructive sleep apnoea.
The syndrome typically begins around menarche but may appear later in life especially in women who experience weight gain.
PCOS is to be suspected in women with one or more of the following :
Oligomenorrhoea/amennorhoea
Subfertility/infertility
Hirsutism/acne/androgenic alopecia
Incidental sonologic detection of “polycystic” ovaries]
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Polycystic Ovarian Syndrome. Following are the major recommendations :
Case definition:
A universally accepted definition has been lacking. It is currently diagnosed by applying the diagnostic criteria proposed at the 2003 Rotterdam international consensus conference. As PCOS is a syndrome, it is defined by a combination of features rather than any one single manifestation.
It is also a diagnosis of exclusion. Other conditions which can mimic PCOS by causing menstrual irregularity and/or hyperandrogenism must be excluded.
Incidence of The Condition In Our Country
The prevalence in the west is between 5-7% and increasing with the trend of increasing obesity. The prevalence in our country is undetermined but is a common condition encountered in practice specially by endocrinologists, gynaecologists and dermatologists.
Differential Diagnosis
Non classic congenital adrenal hyperplasia
Cushing’s syndrome
Primary hypothyroidism
Hyperprolactinemia
Acromegaly
Virilising adrenal and ovarian tumour
Drugs
Prevention And Counseling
The only mode of prevention is prevention of obesity. Women with PCOS need to be counseled about the condition itself along with its associations, specially metabolic and cardiovascular. A properly informed patient would be better equipped to choose between different modalities of treatment, especially in case of hirsutism.
Optimal Diagnostic Criteria, Investigations, Treatment & Referral Criteria
Clinical Diagnosis
The current definition of PCOS is the one that was evolved in 2003 at the Rotterdam ESHRE/ASRM-sponsored PCOS consensus workshop. According to this definition PCOS can be diagnosed if ANY two out of the three features mentioned below are present, and other mimicking conditions (e.g. congenital adrenal hyperplasia, androgen-secreting tumours, Cushing's syndrome) have been excluded:
- Oligo- and/or anovulation
- Clinical and/or biochemical signs of hyperandrogenism
- Polycystic ovaries
It is a condition arising out of functional abnormalities of the ovaries and the documentation of polycystic ovaries is not an essential criterion. By the same token, the presence of polycystic ovaries alone does not suffice to make the diagnosis.
History and physical examination is important to determine the presence of features of the syndrome, their temporal profile, and relevant family history. Clinical clues to ascertain likelihood of other mimicking medical conditions are to be looked for. Similarly clinical evaluation should also focus on the possibilities of other known associations of PCOS.
Clinical Features of PCOS :
- Oligo- and/or anovulation oligomenorrhoea (i.e.fewer than 9 menstruations in a year) amenorrhoea dysfunctional uterine bleeding subfertilty /infertility.
- Hyperandrogenism hirsutism acne male pattern alopecia
Associations of PCOS:
- Metabolic syndrome and insulin resistance obesity hypertension acanthosis nigricans
- Sleep apnoea excessive snoring and daytime sleepiness
Differential diagnosis of PCOS :
- Non-classic CAH: family history of infertility, hirsutism or both
- Cushing’s syndrome: Hypertension, striae, easy bruising
- Hyperprolactinemia : Galactorrhoea
- Primary hypothyroidism : Goitre, other clinical features
- Acromegaly : Acral enlargement, coarse features, prognathism
- Virilising adrenal/or ovarian neoplasm : clitorimegaly, extreme hirsutism and malepattern baldness, abdominal/pelvic mass
- Drug history for exposure to androgens, anabolic steroids, valproic acid, cyclosporine
Investigations:
To confirm diagnosis :
i) Ultrasound of ovaries.
Regularly menstruating women should be scanned in the early follicular phase (cycle days 3-5). Oligo-/amenorrhoeic women should be scanned either at random or between days 3 and 5 after a progestin-induced withdrawal bleeding. Presence of 12 or more follicles, measuring 2-9 mm in diameter in either ovary, and/or increased ovarian volume (>10ml) is consistent with the diagnosis. Whenever feasible, transvaginal approach should be used specially in obese individuals.
ii) Serum testosterone.
It should be measured in the morning preferably in the follicular phase. A level in the upper normal range or slightly elevated is generally seen in PCOS. A level in the range of normal adult males is suggestive of virilising disorders. If total testosterone is normal, a reliable free testosterone level if available should be asked for.
For differential diagnosis :
i) TSH
TSH should be measured to rule out primary hypothyroidism. Hypothyroidism can cause ovulatory dysfunction but not significant hyperandrogenism. Therefore the role of measuring TSH in women with significant hyperandrogenism is to rule out a chance coexistence of a common disorder responsible for ovarian dysfunction and subfertility.
ii) Prolactin
Prolactin levels should be measured in the fasting state in the morning to rule out hyperprolactinemia resulting from prolactionomas. Like hypothyroidism, hyperprolactinemia can cause ovulatory dysfunction but not significant hyperandrogenism. Importantly, many patients with PCOS may have prolactin levels in the upper normal range or slightly elevated and, therefore, this should not be considered indicative of prolactinomas.
iii) Gonadotropins and Estradiol
Measurement of FSH and LH levels is not required for diagnosis of PCOS These are useful for differential diagnosis in the group of females with oligo- or anovulation without features of hyperandrogenism, namely :
- Pre mature ovarian failure (high FSH/LH)
- Hypogonadotropic hypogonadism (normal/low FSH/LH and low estradiol).
PCOS, in contrast, has normal FSH, with or without elevated LH, and normal estradiol
iv) Serum 17-hydroxyprogesterone
This is to be measured in the follicular phase of menstrual cycle in the morning only in those in whom non-classic CAH is considered to be a possibility.
v) Serum DHEAS
In those whom virilising adrenal neoplasms need to be ruled out.
vi) Tests for acromegaly and Cushing’s syndrome need to be done only in those with suspicious clinical features.
Ancillary Studies to look for associations of PCOS :
- Oral Glucose Tolerance Test
- Fasting Lipid Profile
- Polysomnography
Only when there is a suspicion of sleep apnoea
Treatment:
Treatment choice depends on the component of the condition which is desired to be addressed in a given clinical situation.
Applicable to all :
i) Weight loss in those overweight.
All overweight/obese individuals with PCOS, weight reduction is recommended. A 5-7 % weight loss can help improve Insulin resistance and thereby improve ovulatory dysfunction, hyperandrogenism, metabolic abnormalities
ii) Metformin
By reducing hepatic glucose output reduces insulin levels and can have a wide effect like weight loss. Effect of metformin is evident regardless of baseline body weight.
Applicable to those with menstrual irregularity and desire to conceive:
- Metformin
- ovulation induction with antiestrogens (clomiphene) or aromatase inhibitor (lerotrozole), or gonadotropins Metformin can be used in combination with other ovulation inducing agents.
Applicable to those needing treatment for menstrual irregularity alone :
- cyclical progesterone
- OCPs
Applicable to those needing treatment for hirsutism :
- Cosmetic measures (bleaching, waxing, shaving, chemical depilation)
- Permanent hair reduction (electrolysis, photoepilation)
- Pharmacologic therapy (not for those desiring/likely to conceive) OCPs
- Antiandrogens (spironolactone) and 5 alpha reductase inhibitor (finasteride)
OCPs are commonly combined with antiandrogens
Standard operating procedure
Consider PCOS in women with hirsutism and/or other cutaneous markers of hyperandrogenism, oligo- or amenorrhoea, subfertility.
- Rule out pregnancy in amenorrhoeic women.
- Check testosterone level
- Pelvic sonography
- Exclude other conditions mimicking PCOS to confirm diagnosis of PCOS. Choice of test would depend on the clinical situation. TSH and prolactin should be checked in all those with menstrual irregularity and/ or infertility.
- Check for associated features of metabolic syndrome – including glucose intolerance and dyslipidemia.
- Consider possibility of sleep apnoea
- Insulin resistance reduction with weight loss (in those overweight) and metformin can help ameliorate all features
- For oligo- or amenorrhoea : cyclic OCPs or progestin alone
- For hirsutism : cosmetic measures along with pharmacologic therapy and/or electrolysis/photoepilation
- For infertility : metoformin and/or other ovulation induction measures
Referral criteria:
- When endocrinological conditions like acromegaly, Cushing’s syndrome, virilising conditions and non-classic CAH are suspected or diagnosed and appropriate endocrinologic and surgical services are not available.
- Infertile women needing ovulation induction with complex regimen if experience with the same is not available.
- Assisted reproduction services.
Guidelines by The Ministry of Health and Family Welfare :
Dr Sailesh Lodha
Fortis Escorts Jaipur

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd