- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
POEM has higher treatment success than pneumatic dilation for achalasia
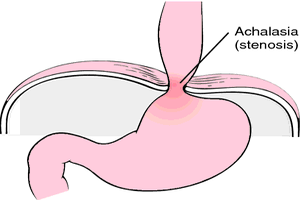
Delhi: Peroral endoscopic myotomy (POEM) can be considered as an initial treatment option for patients with oesophagal achalasia alternative to pneumatic dilation, according to a recently published study in the journal JAMA.
The study found that treatment-naive patients with achalasia, when treated with POEM, had a significantly higher treatment success rate at 2 years compared with pneumatic dilation, at 92% versus 54%, respectively.
Achalasia is an oesophagal motor disorder, with a rare occurrence of approximately 10 cases per 100 000 adults. It is characterized by progressive degeneration of ganglion cells in the myenteric plexus of the oesophagus leading to insufficient swallow-induced relaxation of the lower oesophagal sphincter (LES) and absence of peristalsis along the oesophagal body. This results in impaired passage of food from the oesophagus to the stomach causing symptoms of liquid and solid food dysphagia, regurgitation, chest pain, pulmonary complications, and weight loss.
Fraukje A. Ponds, University of Amsterdam, Amsterdam, the Netherlands, and colleagues compared the effects of POEM vs pneumatic dilation as initial treatment of treatment-naive patients with achalasia.
The trial enrolled 130 previously untreated patients from six centres in the Netherlands, Germany, Italy, Hong Kong, and the U.S. Patients during the period of September 2012 to July 2015. The patients had a mean age of 48.6 years, 56% were men, and participants were followed for 2 years after initial treatment.
The primary outcome was treatment success (defined as an Eckardt score ≤3 and the absence of severe complications or re-treatment) at the 2-year follow-up.
64 patients were randomized to receive POEM whereas 66 received pneumatic dilation, 126 patients (95%) completed the trial. Following were the findings of the researchers following trial completion:
- The primary outcome of treatment success occurred in 58 of 63 patients (92%) in the POEM group vs 34 of 63 (54%) in the pneumatic dilation group, a difference of 38%.
- Of the 14 prespecified secondary endpoints, no significant difference between groups was demonstrated in 10 endpoints.
- There was no significant between-group difference in median integrated relaxation pressure (9.9 mm Hg in the POEM group vs 12.6 mm Hg in the pneumatic dilation group; difference, 2.7 mm Hg or median barium column height (2.3 cm in the POEM group vs 0 cm in the pneumatic dilation group; difference, 2.3 cm.
- Reflux esophagitis occurred more often in the POEM group than in the pneumatic dilation group (22 of 54 [41%] vs 2 of 29 [7%]; difference, 34%.
- Two serious adverse events, including 1 perforation, occurred after pneumatic dilation, while no serious adverse events occurred after POEM.
"These findings support consideration of POEM as an initial treatment option for patients with achalasia," wrote the researchers.
"Although POEM is more invasive and requires more technical endoscopic skills, the risk of severe complications was not higher than with pneumatic dilation, especially when performed by experienced endoscopists," the authors noted.
"POEM's acceptance as a first-line therapy may depend not only on longer follow-up to assess the durability of response but also, in part, on whether the reimbursement value of this procedure is acknowledged to be more similar to a surgical intervention than a minimally invasive endoscopic intervention," Brian C. Jacobson, and David R. Lichtenstein, of Boston University School of Medicine, said in an accompanying editorial.
To read the complete study log on to doi:10.1001/jama.2019.8859

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd