- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Pharmacological treatment must in older adults if SBP persistently ≥150 mm Hg
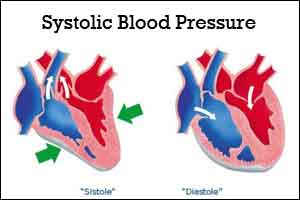
This joint guideline presents evidence on benefits and harms of treating to higher versus lower systolic blood pressure (SBP) targets in older adults (age, ≥60) with hypertension. Recommendations are based on a systematic review of randomized controlled trials (for primary outcomes) and observational studies (for harms). One of the main recommendations is to initiate treatment in older adults with SBP persistently ≥150 mm Hg to achieve a target SBP of <150 mm Hg.
Key Findings
- All studies showed benefit for hypertension treatment in older adults, most of whom had baseline SBPs >160 mm Hg.
- With absolute risk reductions (ARRs) expressed as percentage points and adjusted to 5-year time frames, high-quality evidence showed lower all-cause mortality (ARR, 1.64), stroke incidence (ARR, 1.13), and adverse cardiac events (ARR, 1.25) in patients with baseline SBPs ≥160 mm Hg who were treated to achieve SBPs <150 mm Hg.
- In studies with lower SBP targets (<140 mm Hg) compared with higher targets, low-quality evidence showed no significant relative reductions in all-cause mortality or adverse cardiac events, whereas moderate-quality evidence showed lower risk for stroke (ARR, 0.49). However, many of these studies did not achieve target BPs and failed to show significant BP differences between the intensive treatment and control arms, so they might have been unable to show a difference in clinical outcomes.
- In patients with histories of stroke or transient ischemic attack (TIA), moderate-quality evidence suggested that treating to SBP of 130 mm Hg to 140 mm Hg lowered risk for stroke recurrence (ARR, 3.02) but not for adverse cardiac events or all-cause death.
- Evidence was insufficient to evaluate the benefit of treating patients who have isolated diastolic hypertension.
- With regard to harms, low-quality evidence suggested that treating to lower BP targets (achieved SBP range, 121.5−143 mm Hg) heightened risk for syncope.
Recommendations
- Initiate treatment in older adults with SBP persistently ≥150 mm Hg to achieve a target SBP of <150 mm Hg (strong recommendation, high-quality evidence).
- In older adults with previous stroke or TIAs, consider treating to <140 mm Hg to lower risk for recurrence (weak recommendation, moderate-quality evidence).
- In older adults at high cardiovascular (CV) risk, consider treating to <140 mm Hg to lower risk for stroke or adverse cardiac events (weak recommendation, low-quality evidence). Patients at high CV risk include those with known vascular disease, most patients with diabetes, patients with chronic kidney disease (CKD), patients with metabolic syndrome or 10-year CVD risk ≥15%, and older patients (age, ≥75).
For more details click on the following link: http://www.jwatch.org/na43262/2017/03/02/pharmacologic-treatment-hypertension-older-adults
chronic kidney diseaseHypertensionPharmacologic treatmentstrokesystolic blood pressuretransient ischemic attack
Next Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd