- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
PGI Doctors report a classical case of Bitot’s Spots
Dr.Jagat Ram and colleagues at Post Graduate Institute of Medical Education and Research, Chandigarh, India have reported a classical case of Bitot’s Spots which has appeared in NEJM.
Vitamin A deficiency (VAD) can cause a range of ocular manifestations, known collectively as xerophthalmia, including night blindness, conjunctival and corneal xerosis, and keratomalacia, and is an important cause of preventable blindness.Bitot’s spots, first described by the French physician Pierre Bitot in 1863 in debilitated children, are an important sign for diagnosing vitamin A deficiency (VAD). Bitot’s spots are typically dry-appearing triangular patches of xerosed conjunctiva with a layer of foam on the surface, usually located temporal to the cornea .
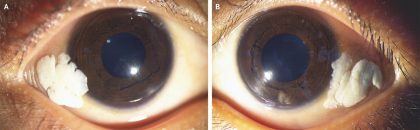
According to the history ,a 4-year-old boy was brought by his father to the ophthalmology department of PGI with a 1-year history of enlarging white deposits in both eyes with decreased night vision. When doctors examined him they found that the conjunctivae of both the right eye (Panel A) and the left eye (Panel B) appeared dry and wrinkled, with foamy, cream-coloured deposits near the outer corners. In addition the corneas were clear, the fundi were normal, and the visual acuity was 20/30 in both eyes. The child was pale, with hypopigmented hair, a weight of 10.5 kg (z score of less than −3), and a height of 92 cm (z score of −2.8).
The ocular findings were consistent with Bitot’s spots, which are accumulations of keratin, often intermixed with an overgrowth of Corynebacterium xerosis, that results from epithelial metaplasia caused by vitamin A deficiency. Vitamin A deficiency can also cause blindness, as a result of corneal ulceration with scarring, and particularly night blindness, as a result of dysfunction of rod photoreceptor cells.
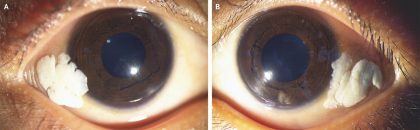
Courtesy NEJM
In this patient, the serum vitamin A level was 16.8 μg per deciliter (0.59 μmol per litre) (reference range, 20 to 40 μg per deciliter [0.70 to 1.40 μmol per litre]), and the retinol-binding protein level was 0.01 g per litre (reference range, 0.03 to 0.06). Further history taking revealed extreme poverty, and further examination showed signs of dietary deficiency, with no evidence of intestinal parasites. The patient received an oral dose of vitamin A, which was repeated 4 weeks later. Artificial tears were also administered. The Bitot’s spots abated, although they did not completely resolve, over the course of 12 weeks. The parents were advised to administer another dose of vitamin A every 6 months until the child was 5 years of age.
High-dose vitamin A is the treatment for all individuals with xerophthalmia and for infants or children with severe malnutrition or measles.Improvement of Bitot’s spots is seen within 2 weeks of high-dose vitamin A therapy.
For more details click on the link: DOI: 10.1056/NEJMicm1715354

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd