- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
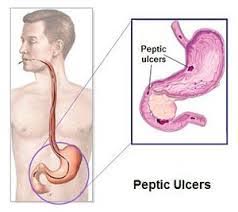
Peptic Ulcer Perforation - Standard Treatment Guidelines
Lau and Leow have indicated that perforated peptic ulcer was clinically recognized by 1799, but the first successful surgical management of gastric ulcer was by Ludwig Heusner in Germany in 1892. In 1894, Henry Percy Dean from London was the first surgeon to report successful repair of a perforated duodenal ulcer. Wangensteen et al reported that in a patient with perforation but without evidence of pneumoperitoneum, one can safely assume that perforation has sealed off on its own. They advocated a nonoperative approach for such patients. However, they too supported operative treatment in patients with perforated ulcer and evidence of pneumoperitoneum.
Berne and Donovan emphasized the use of a water-soluble upper GI study to demonstrate spontaneous sealing of the perforation. They demonstrated that as many as 40% of perforated peptic ulcers had no evidence of leak on upper GI contrast studies. Berne and Donovan concluded that these patients can be observed safely as long as peritonitis does not develop. Mortality rates were 6% and 3% in the operative and nonoperative groups, respectively.
Donovan et al proposed dividing patients based on their Helicobacter pylori infection status and recommended nonoperative treatment in all patients except those without H pylori infection and those in whom prior treatment of H pylori infection had failed.
Despite strong arguments favoring nonoperative treatment of patients with perforated PUD, delaying the initiation of surgery more than 12 hours after presentation was demonstrated to worsen the outcome. Therefore, when definitely indicated, a laparotomy should be performed as soon as possible.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Peptic Ulcer Perforation. Following are the major recommendations :
Indian Incidence
There are no statistics available on this topic.
Symptoms
- Sudden, sharp and severe pain in upper abdomen
- Spreading of pain to rest of abdomen
- Pain gets worse after oral ingestion or movements
- Feeling of giddiness and fainting
- Fever
- Weakness
Signs
Tachycardia
Fever
Pallor
Reduced abdominal wall movements
Complications
Investigations
- Haemogram
- Liver Function Tests
- Blood sugar
- Serum creatinine
- Bleeding time, clotting time and prothrombin time
- Xray chest
- ECG
- USG abdomen
- Upper GI endoscopy
Management
Resuscitation
Fluid resuscitation should be initiated as soon as the diagnosis of peptic ulcer disease (PUD) is made. Essential steps include insertion of a nasogastric tube to decompress the stomach and a Foley catheter to monitor urine output. Intravenous infusion of fluids is begun, and broad-spectrum antibiotics are administered. In select cases, insertion of a central venous line or a Swan-Ganz catheter may be necessary for accurate fluid resuscitation and monitoring. As soon as the patient has been adequately resuscitated, emergent exploratory laparotomy should be performed.
Conservative Treatment
Wangensteen et al reported that in a patient with perforation but without evidence of pneumoperitoneum, one can safely assume that perforation has sealed off on its own. They advocated a nonoperative approach for such patients. However, they too supported operative treatment in patients with perforated ulcer and evidence of pneumoperitoneum.
Berne and Donovan emphasized the use of a water-soluble upper GI study to demonstrate spontaneous sealing of the perforation. They demonstrated that as many as 40% of perforated peptic ulcers had no evidence of leak on upper GI contrast studies. Berne and Donovan concluded that these patients can be observed safely as long as peritonitis does not develop. Mortality rates were 6% and 3% in the operative and nonoperative groups, respectively.
Donovan et al proposed dividing patients based on their Helicobacter pylori infection status and recommended nonoperative treatment in all patients except those without H pylori infection and those in whom prior treatment of H pylori infection had failed.
Despite strong arguments favoring nonoperative treatment of patients with perforated PUD, delaying the initiation of surgery more than 12 hours after presentation was demonstrated to worsen the outcome. Therefore, when definitely indicated, a laparotomy should be performed as soon as possible
Surgical Treatment
The appropriate surgical procedure depends on the location and nature of the ulcer. Many authorities recommend simple oversewing of the ulcer, with treatment of the underlying H pylori infection or cessation of nonsteroidal anti-inflammatory drugs (NSAIDs) for bleeding PUD. Additional surgical options for refractory or complicated PUD include vagotomy and pyloroplasty, vagotomy and antrectomy with gastroduodenal reconstruction (Billroth I) or gastrojejunal reconstruction (Billroth II), or a highly selective vagotomy.
The patient is placed in the supine position. A midline incision provides the most expeditious entry into the abdominal cavity. The incision can be extended to the symphysis pubis if necessary.
Once the abdomen is entered, the stomach and duodenum are carefully examined to determine the site of perforation. If the anterior surfaces of the stomach and duodenum show no abnormalities, the gastrocolic ligament is serially divided between clamps to allow entrance into the lesser sac and inspection of the posterior surface of the stomach.
The choice of operative procedure depends on variables such as the presence of shock, the presence of life-threatening comorbid conditions, the degree of contamination of the upper abdomen, the amount and duration of perforation, and whether the patient has a history of, or currently has intraoperative evidence of, chronic peptic ulceration.
In the presence of life-threatening comorbid conditions and severe intra-abdominal contamination, the safest technique for an acute anterior duodenal perforation is a simple closure with a Graham patch, using omentum. Several full-thickness simple sutures are placed across the perforation, using 2-0 or 3-0 silk sutures. A segment of omentum is placed over the perforation. The silk sutures are secured.
If contamination of the upper abdomen is minimal and the patient is stable, a definitive ulcer procedure can be performed. For a perforated duodenal ulcer, this may include a highly selective vagotomy, a truncal vagotomy and pyloroplasty, or vagotomy and antrectomy.
For a perforated gastric ulcer, the procedure performed depends on the patient's condition. If the patient is moribund, the ulcer is best excised by grasping it with multiple Allis clamps and using a linear stapler. Alternatively, the ulcer can be excised with electrocautery; the defect is approximated with a 2- layer closure with inner continuous 3-0 absorbable sutures and outer interrupted Lambert sutures using 2-0 or 3-0 silk sutures.
In a stable patient, the ulcer is excised and sent for frozen section analysis to exclude malignancy. For a benign gastric ulcer, a distal gastrectomy with either a Billroth I gastroduodenostomy or a Billroth II gastroduodenostomy is performed.
Post Operative Care & Complications
The nasogastric tube can be discontinued on postoperative day 2 or 3, depending on the return of GI function, and diet can be slowly advanced. Patients who are found to have H pylori infection should receive the appropriate antibiotic regimen. Patients with high serum gastrin levels should undergo an evaluation for Zollinger-Ellison syndrome. Patients should undergo upper endoscopy to evaluate the area of ulcer and healing of the perforation site 4-6 weeks after surgery.
Surgical complications include pneumonia (30%), wound infection, abdominal abscess (15%), cardiac problems (especially in those >70 y), diarrhea (30% after vagotomy), and dumping syndromes (10% after vagotomy and drainage procedures).
Referral Criteria
- ICU care may be needed in patients who present late with severe sepsis and have other systemic illnesses.
- Patients with recurrence of perforation few days after surgery may need ICU care, parenteral nutrition, investigations for gastrinoma and further surgery.
Medicolegal
- Failure to detect / investigate or refer a patient of suspected peptic ulcer perforation.
- Delay in treatment.
- Delay in diagnosing complications and taking corrective action.
WHO DOES WHAT?
Doctor:
- Surgeon: diagnosis & work up
Pre operative planning
Operative procedure
Post operative follow up
- Anesthetist: PAC, anesthesia, post op ICU management
Nurse
- Dressing of the wound
- Pre & post operative care
Technician
- Pre op equipment and drugs to be checked and kept ready
- Assist anesthetist in the OT
- Assist the surgeon, positioning of the patient
Resources Required For One Patient / Procedure (Patient weight 60 Kgs)
| Human Resources | Investigations | Drugs/Consumables | Equipment' |
| Surgeon – 1 Medical Officer / Assistant Surgeon – 1 Anesthetist – 1 Pathologist – 1 Staff Nurse – 1 Technician – 1 Nursing Orderly – 1 Sweeper – 1 | Haemogram LFT Blood Sugar S. Electrolytes KFT ECG X-Ray – Chest USG Histopathology | Antibiotics Analgesic I.V. Fluids Sutures Drains Catheters Anesthetic drugs Dressings | OT Table & lights Instrument trolley Laparoscopic Surgery set General Surgery Set Cautery Suction Anesthetic Equipment Monitors |
Guidelines by The Ministry of Health and Family Welfare :
Dr. Arun Prasad

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd