- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Pelvic Inflammatory disease-Standard Treatment Guidelines
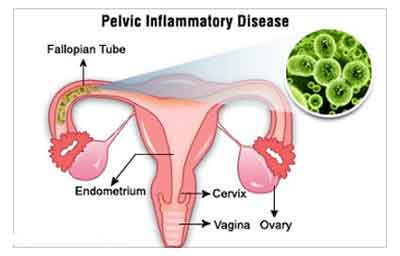
Introduction
Various causative organisms include
- Sexually transmitted organisms, especially N. gonorrhoeae and C. trachomatis,
- Microorganisms that comprise the vaginal flora (e.g., anaerobes, G. vaginalis, Haemophilus influenzae, enteric Gram-negative rods, and Streptococcus agalactiae)2
- Others like: Cytomegalovirus (CMV), M. hominis, U. urealyticum, and M. genitalium associated in some cases.
Ministry of Health and Family Welfare, Government of India has issued the Standard Treatment Guidelines for Pelvic Inflammatory disease (PID).Following are the major recommendations :
Often more than one species from vaginal flora isolated (“polymicrobial” PID). No microorganisms are recovered from 20-30% of patients. A large number of unculturable species which are normal residents of the genital tract may have role to play.
Clinical features
The presentation may be Acute or Chronic.
Important clinical signs and symptoms include
- Vaginal/cervical discharge, congestion or ulcers
- Menstrual irregularities like heavy irregular vaginal bleeding, dysmenorrhoea,
- Dyspareunia, Dysuria or tenesmus
- Temperature> 39 degree C
- Lower abdominal tenderness or guarding
- Uterine/adnexal tenderness, cervical movement tenderness,
- Presence of a pelvic mass
PID can present with a vast array of clinical manifestations
- Salpingitis is the most important feature of PID.
- Infection and inflammation of the endometrium, blood vessels and lymphatics without visually recognized salpingitis.
- None of the symptoms, clinical signs, or laboratory results are pathognomonic for PID. About two-thirds of cases of PID are probably unrecognized.4
- Chronic PID is an even more poorly defined entity used for patients with chronic pain or infertility, caused by pelvic adhesions and other abnormalities from a prior episode
Sequelae
Sequelae are common.
- Tubal infertility due to tubal and peritubal damage
- Ectopic Pregnancy
- Chronic pain and other gynecological morbidity
INCIDENCE OF THE CONDITION IN OUR COUNTRY
The exact incidence of PID is unknown, because the disease cannot be diagnosed reliably from clinical symptoms and signs. Direct visualization of the fallopian tubes by laparoscopy is the best single diagnostic test, but it is invasive, lacks sensitivity, and is not used routinely in clinical practice.
PID is the most common gynaecological reason for admission to hospital in the USA. In resource-poor countries it accounts for 17% to 40% of gynaecological admissions in sub-Saharan Africa, 15% to 37% in Southeast Asia, and 3% to 10% in India (3).
DIFFERENTIAL DIAGNOSIS
- In mild cases
o Rule out various causes of vaginal discharge. - In severe cases
o Rule out causes of acute abdomen, including ectopic pregnancy and acute appendicitis.
o Other gynecological differentials include rupture, bleeding, or torsion of an ovarian cyst, pelvic endometriosis.
o Mesenteric lymphadenitis, regional ileitis, enteritis, and other manifestations of inflammatory bowel disease.
o Urinary tract infection and colic from renal or ureteral stones.
PREVENTION AND COUNSELING
General measures as applicable to all patients with suspected STIs
- Educate and counsel patient and sex partner(s) regarding RTIs/STIs, genital cancers, safer sex practices and importance of taking complete treatment.
- Treat partner(s) for the suspected organisms.
- Advise sexual abstinence during the course of treatment to minimize transmission.
- Promote the use of barrier contraception like condoms, educate about correct and consistent use.
- Refer for voluntary counseling and testing for HIV, Syphilis and Hepatitis B.
- Consider immunization against Hepatitis B.
- Schedule return visit after 7 days to ensure treatment compliance as well as to see reports of tests done.
- If symptoms persist, assess whether it is due to treatment failure or reinfection and advise prompt referral.
OPTIMAL DIAGNOSTIC CRITERIA, INVESTIGATIONS, TREATMENT & REFERRAL CRITERIA
Situation 1: At Secondary Hospital/ Non-Metro situation: Optimal Standards of Treatment in Situations where technology and resources are limited
Clinical Diagnosis
The clinical diagnosis of acute PID is imprecise.
- The PPV of a clinical diagnosis depends on the epidemiologic characteristics of the population. It is higher among sexually active young women (particularly adolescents), patients attending STD clinics, and those who live in other settings where the rates of gonorrhea or chlamydia are high.
- Many episodes of PID go unrecognized. Health-care providers should maintain a low threshold for the diagnosis of PID.
Clinical evaluation is aimed at
- RULING OUT THE NUMEROUS DIFFERENTIALS
- ASSESSING FOR SEVERITY OF DISEASE
RULING OUT THE NUMEROUS DIFFERENTIALS
A simple stepwise algorithm for a patient presenting with abdominal signs and symptoms and vaginal discharges uggestive of Acute PID
1. Pregnancy test:
- If positive points towards Ectopic Pregnancy or other pregnancy complications.
- If negative: then do wet mount or Gram stain of cervical/vaginal secretions.
2. In a Sexually active patient: presence of yellow cervical mucopus or the wet mount revealing WBC’s outnumbering the number of epithelial cells makes PID a probable diagnosis
3. USG and explorative laparoscopy to exclude appendicitis or ruptured abscess. No symptom or sign is pathognomonic of PID. All symptoms have a low positive and negative predictive value for the diagnosis of PID.
ASSESSING FOR SEVERITY OF DISEASE
1. SUBCLINICAL DISEASE (ATYPICAL PID, “SILENT” PID)
2. MILD AND MODERATELY SEVERE PID
3. SEVERE PID
Recommendations for diagnosing PID
Empiric treatment for PID should be initiated in sexually active young women and other women at risk for STDs,
- if there is pelvic or lower abdominal pain (with no other apparent cause)
AND
- if one or more of the following minimum criteria are present on pelvic examination:
a.cervical motion tenderness
OR
b. uterine tenderness
OR
c. adnexal tenderness.
Additional criteria to enhance the specificity of the minimum criteria and support a diagnosis
1. CLINICAL
- oral temperature >101° F (>38.3° C);
- abnormal cervical or vaginal mucopurulent discharge (MPC)
- cervical friability
2. LABORATORY
- presence of abundant numbers of WBC on saline microscopy of vaginal fluid;
- elevated erythrocyte sedimentation rate;
- elevated C-reactive protein
- laboratory documentation of cervical infection with N. gonorrhoeae or C. trachomatis.
Most specific criteria for diagnosing PID include: (NOT ROUTINELY RESORTED TO)
- endometrial biopsy with histopathologic evidence of endometritis
- transvaginal sonography or magnetic resonance imaging techniques showing thickened,
fluid-filled tubes with or without free pelvic fluid or tubo-ovarian complex - Doppler studies suggesting pelvic infection (e.g., tubal hyperemia)
- Laparoscopic abnormalities consistent with PID.
Investigations
LABORATORY TESTS
- Vaginal smear demonstrating
o increase in the inflammatory cells
o presnec of gnid (Gram’s stain)
o organism for BV or trichomoniasis - Raised ESR (>15 mm/h)
- CRP: The mean CRP is 47 mg/L (range 32-63) for mild tubal abnormalities and 83 mg/L (range 65-103) for severe tubal disease.
- Peripheral WBC count (>10,000 mm3)
- Laparoscopy: Gives a more accurate diagnosis of salpingitis and more complete bacteriologic diagnosis. It has been the gold standard to diagnose PID. Criteria used to define salpingitis observed through the laparoscope include tubal erythema, swelling, and exudate. However, not practical and not justified for majority of cases when symptoms are mild or vague.
- Endometrial biopsy: for the outpatient diagnosis of subclinical or silent PID.
- Pregnancy test for all potentially fertile women with acute abdominal/pelvic pain irrespective of contraception use.
- Ultrasound examination: useful noninvasive test to diagnose and follow the course of severe PID.
- Transvaginal ultrasound
- Transvaginal power Doppler sonography
- Testing for N. gonorrhoeae and C. trachomatis: for a more specific diagnosis
- Microscopy and culture of urine
- Culdocentesis (USG guided): Its use has become less common to diagnose PID.
Treatment
- Antimicrobial therapy is required to treat infection present in PID.
- Early antibiotic treatment in the first 3 days reduces tubal infertility
- Choice of antimicrobial is empiric as collection and microbial testing of fallopian-tube specimens is not practical and reports take time in the majority of cases.
- Antimicrobial regimen must cover at least the most frequently expected microbes i.e N. gonorrhoeae, C. trachomatis, and common aerobic and anaerobic isolates.
- At least two drugs are recommended for syndromic treatment of PID.
- Treatment should be initiated as soon as the presumptive diagnosis has been made because prevention of long-term sequelae is dependent on early administration of appropriate antibiotics.
Treatment
Outpatient treatment
In mild or moderate PID
- Tab. Cefixime 400 mg orally BD for 7 days
PLUS - Tab. Metronidazole 400mg orally, twice daily for 14 days
PLUS - Tab Doxycycline, 100mg orally, twice a day for 2 weeks
Adjunctive treatment
- Tab. Ibuprofen 400mg orally, three times a day for 3-5 days
- Tab. Ranitidine 150mg orally, twice daily to prevent gastritis
- Remove intra uterine device, if present, under antibiotic cover of 24-48 hours
- Advise abstinence during the course of treatment and educate on correct and consistent use of condoms
Follow up
- Observe for 3 days, if no improvement i.e.o Fever persists
o No reduction in abdominal tenderness
o No reduction in cervical movement, adnexal and uterine tenderness
o If symptoms worsen
Refer for inpatient treatment
- Repeat testing of all women who have been diagnosed with chlamydia or gonorrhea is recommended 3–6 months after treatment, regardless of whether their sex partners were treated
Syndrome specific guidelines for partner management
- Treat all partners in past 2 months
- Treat male partners for urethral discharge (Refer Guidelines)
- Advise sexual abstinence during the course of treatment
- Provide condoms, educate on correct and consistent use
- Refer for voluntary counseling and testing for HIV, Syphilis and Hepatitis B
- Inform about the complications if left untreated and sequelae
- Schedule return visit after 3 days, 7 days and 14 days to ensure compliance
Prevention
- Screening and treating sexually active women for chlamydia
- Whether the incidence of PID can be reduced by identifying and treating women with BV is unclear.
Inpatient Treatment
Guidelines for the hospitalization of patients
- If no response; poor response to treatment; or worsening within 48-72 hrs
- Severe PID or signs of prostration, signs of peritonitis, septicaemia, nausea and vomiting, or high fever.
- Surgical emergencies (e.g., appendicitis) cannot be excluded;
- Patient is pregnant;
- Patient unable to follow or tolerate an outpatient oral regimen
- Tubo-ovarian abscess.
Recommended Parenteral Treatment
Inj. Cefotetan 2 g IV every 12 hourly (better coverage against anaerobes)
OR
Inj. Cefoxitin 2 g IV every 6 hour (better coverage against anaerobes)
PLUS
Tab. Doxycycline 100 mg orally or IV every 12 hours (Preferably orally because of pain associated with intravenous infusion).
- Clinical experience to guide decisions regarding transition to oral therapy.
- Usually can be shifted within 24–48 hours of clinical improvement.
- Oral therapy with doxycycline (100 mg twice a day) should continue to complete 14 days of therapy.
Alternative Regimes
- Other second- or third-generation cephalosporins (e.g., ceftizoxime, cefotaxime, and ceftriaxone) WITH Doxycycline. Effective therapy for PID but are less active than cefotetan or cefoxitin against anaerobic bacteria.
- Inj. Clindamycin 900 mg IV every 8 hours WITH Inj. Gentamicin loading dose IV or IM (2 mg/kg of body weight), followed by a maintenance dose (1.5 mg/kg) every 8 hours Then Shift to Ongoing oral therapy with Tab. doxycycline 100 mg orally twice a day OR Tab Clindamycin 450 mg orally four times a day to complete a total of 14 days of therapy.
- Inj. Azithromycin for 1 week (500 mg IV for 1 or 2 doses followed by 250 mg orally for 5– 6 days) WITH 12-day course of metronidazole.
- Inj. Ceftriaxone 250 mg IM in a single dose WITH Tab. Doxycycline 100 mg orally twice a day for 14 days WITH or WITHOUT Metronidazole 500 mg orally twice a day for 14 day (better coverage against N. gonorrhoeae.
- Inj. Cefoxitin 2 g IM in a single dose and Probenecid, 1 g orally administered concurrently in a single dose WITH Tab Doxycycline 100 mg orally twice a day for 14 days WITH or WITHOUT Tab Metronidazole 500 mg twice a day for 14 day
- If the culture for gonorrhea is positive, treatment should be based on results of antimicrobial susceptibility.
Special Considerations
Pregnancy
- High risk for maternal morbidity and preterm delivery
- Suspected PID should be hospitalized, treated with parenteral antibiotics.
- Doxycycline is contraindicated in pregnancy.
- Metronidazole is not recommended during the first three months. However, not to be withheld for a severely acute PID, which represents an emergency.
HIV Infection
- Standard parenteral and oral antibiotic regimens
- Microbes like M. hominis, candida, streptococcus apart from HPV infections and related cytologic abnormalities may be associated.
Intrauterine Contraceptive Devices
- Risk for PID confined to the first 3 weeks after insertion
- Insufficient evidence to recommend removal of IUDs in women with acute PID.
- Caution to be exercised if the IUD remains in place, close clinical follow-up is mandatory.
Referral criteria
- The diagnosis is uncertain
- Surgical emergencies e.g. appendicitis or ectopic pregnancy cannot be excluded
- A pelvic abscess is suspected
Situation 2: At Super Specialty Facility in Metro location where higher-end technology is available
Clinical Diagnosis
Same as above
Investigations
Same as above
Plus
- Cervical secretion or urine can be tested with NAAT (for N. gonorrhoeae or C. trachomatis): a positive test for either strongly increases the probability of PID.
- Newer diagnostic techniques, such as PCR and antigen detection assays.
Treatment
Same as above
PLUS
For Tubo-Ovarian Abscess
- At least 24 hours of direct inpatient observation is recommended.
- Initial parenteral therapy with Inj. Ampicillin/Sulbactam 3 g IV every 6 hour WITH Tab Doxycycline 100 mg orally or IV every 12 hour
OR - Ampicillin/sulbactam plus doxycycline is effective against C. trachomatis, N. gonorrhoeae, and anaerobes in women with tubo-ovarian abscess.
- Clindamycin should be continued for oral therapy rather than doxycycline, because clindamycin provides more effective anaerobic coverage.
Standard Operating procedure
- In Patient
- Out Patient
- Day Care
Guidelines by The Ministry of Health and Family Welfare :
Dr. M.K. Daga
Department of Medicine
Maulana Azad Medical College
New Delhi

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd