- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
PAT flap technique aesthetic -it camouflages tip grafts in Rhinoplasty
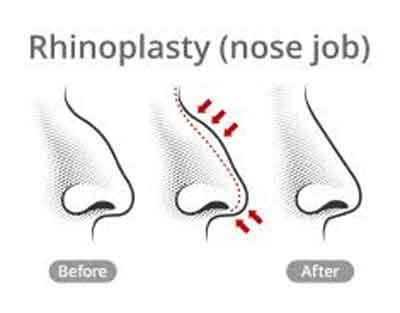
Rhinoplasty, commonly known as a nose job, is a plastic surgery procedure for correcting and reconstructing the form, restoring the functions and aesthetically enhancing the nose by resolving nasal trauma, congenital defect, and respiratory impediment.
Two of the most tricky rhinoplasty complications are tip irregularities and tip graft visibility. In thin-skinned patients, even regular dome sutures can create visible tip irregularities. In thick-skinned patients, strong tip grafts to achieve projection and definition can become visible in long-term follow-up. Common tip camouflage materials are crushed cartilage, temporalis fascia, dorsal rasp leftovers, and acellular dermis, but an ideal graft is still yet to be described.
Courson and Adamson described the intercrural fascia graft, the soft tissue between the medial crura and the domes of the lower lateral cartilages, as a graft to camouflage small irregularities at the end of the rhinoplasty.
According to the author, during the past 3 years, they have been systematically using the same fibrous tissue between the medial crura to cover and camouflage tip grafts as a vascularized advancement flap (not as a graft for premaxillary augmentation. The technique was named the PAT flap (protection of augmented tip) and was used to prevent tip grafts from creating irregularities in the long term and to smooth the infratip lobule transition.
Briefing about the surgical technique the author said that after the tip cartilage is exposed by an open approach, the intercrural soft tissue is identified. Laterally retracting the lower lateral cartilages with a single hook, the dissection begins at the domes and is directed posteriorly to the anterior septal angle at an avascular plane up to the anterior nasal spine, releasing the soft tissue of the intermediate and medial crura. The blood supply is preserved and the flap, now totally freed from the lower lateral cartilages and caudal septum, is hidden at a premaxilla pocket.
After the insertion of the tip grafts, the flap is advanced, covering the graft’s edges and giving a smooth contour to the tip and infratip transition. A 5-0 polydioxanone suture is used to secure the vascularized flap to the grafts.
After that a flap is created dissection is done between the medial crura fibrous tissue and then sutured over the tip grafts, protecting the augmented tip from long-term irregularities. The dissection of the intercrural soft tissue is a necessary step to refine the nasal tip and to allow maneuvers to structure the tip as the tongue-in-groove. Therefore, the manufacture and preservation of the tissue to be used afterward do not add time to the overall procedure. Thick-skinned patients tend to have a thicker intercrural fibrous tissue, favoring its use to cover the strong grafts used to achieve tip projection and definition. However, thinner PAT flaps are available in thin-skinned patients but the use of this technique is essential to cover dome sutures or even small tip graft irregularities.
The author said that during the past 3 years, they have been using the PAT flap instead of a free graft in 35 patients. In 23 (66%) patients, the flap was used to cover tip grafts, and in 12 (34%), to cover newly created domes in thin-skinned patients. No complications were identified such as resorption, graft visibility, or prolonged edema in a 1-year follow-up. A vascularized flap is used to prevent tip irregularities and smooth infratip lobule transition.
The author concluded that the PAT flap has become a common step of primary rhinoplasty when the use of tip augmentation grafts is planned.
For more reference log on to the journal

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd