- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Novel measure for better anaesthesia management
Chicago : A novel measure for assessing the body’s response to surgery may allow for better anesthesia management in the O.R., less pain when regaining consciousness from anesthesia and better postoperative outcomes. According to a study published in the Online First edition of Anesthesiology, the official medical journal of the American Society of Anesthesiologists (ASA), the measure, called the nociception (pain) level index, allowed physicians to more accurately evaluate responses to painful stimulation in patients under general anesthesia, compared to traditional measures.
“There’s currently no standardized, objective method for physicians to monitor the effectiveness of pain relieving drugs being administered during surgery,” said Ruth Edry, M.D., lead study author and senior physician anesthesiologist at Rambam Medical Center in Haifa, Israel. “Not effectively monitoring bodily responses to painful stimulation can lead to insufficient amounts of pain medication being administered, which can result in the patient having severe pain upon regaining consciousness from anesthesia, while too much medication may cause other side effects such as nausea and vomiting or respiratory complications.”
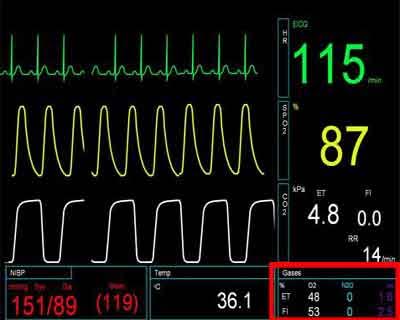
Under general anesthesia, patients are unconscious, but their body still shows reflex responses to the surgical procedure, including changes in heart rate, blood pressure, eyes tearing or sweating. These unwanted reflexes can in some cases be dangerous, and physician anesthesiologists adjust the amount of anesthesia and pain medication when they occur. The nociception (pain) level index, which uses an algorithmic combination to process multiple hormonal and neurological reactions, aims to provide a better, earlier measure of the body’s reflex response to painful stimulation during surgery, compared to the traditional monitoring of individual factors such as changes in heart rate or blood pressure.
In the study, 58 patients who had general anesthesia for a variety of different surgical procedures were examined. Routine anesthesia monitoring was supplemented with a pain monitoring device (PMD-100; Medasense Biometrics; Ramat-Gan, Israel), which generated the nociception (pain) index. The patients’ index was compared to individual, more traditional measures, including heart rate and blood pressure. This index was assessed at several stages including intubation and skin incision, which were designated “noxious” stimuli that would be painful in the conscious person, and where then compared to other non-painful periods.
Compared to other accepted monitors for measuring the body’s response to painful stimulation during surgery, the nociception (pain) index better discriminated presumed pain-causing stimuli from non-pain-causing stimuli. The index also accurately quantified the body’s response to increasingly more painful stimulation, with high sensitivity and specificity, as well as showed a decrease when pain medication was administered.
“Our results demonstrate the superiority of combining multiple physiologic measures over any individual parameter in the evaluation of the body’s response to pain during surgery,” said Dr. Edry. “The article presents an effective index for trending the body’s response to painful stimulation in the anesthetized patient. Once in clinical practice, we can conduct large-scale studies to better assess the influence of this monitor on patient outcomes.”
The study, “Preliminary Intraoperative Validation of the Nociception Level Index,” was supported, in part, by Medasense Biometrics (Ramat-Gan, Israel), the developer of the nociception level index. Dr. Edry and co-author Daniel Sessler, M.D., serve on an advisory board for Medasense and have an equity interest in the company.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd