- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Noninvasive Treatments of low back pain: ACP Guideline
The American College of Physicians (ACP) developed a guideline to present the evidence and provide clinical recommendations on noninvasive treatment of low back pain that has appeared in Annals of Internal Medicine.
Low back pain also known as lumbago is defined as a common, painful condition affecting the lower portion of the spine. The prevalence of low backache is reported to range between 51% and 84%, with most individuals experiencing this condition at some point in their lifetime. Approximately 90% of all low backache will resolve within 6 weeks, with more than 80% of cases resolving within 2 weeks.
Classification of low back pain
- Acute low back pain, which is pain lasting up to 4 weeks, is usually nonspecific and has no underlying condition as an identified cause. Acute low back pain is usually self-limited and resolves on its own with nonpharmacologic treatment.
- Subacute low back pain may persist for 4 to 12 weeks and may require pharmacologic therapy.
- Chronic low back pain-Unresolved low back pain, which is pain lasting longer than 12 weeks, is classified as chronic.
- Given that most patients with acute or subacute low back pain improve over time regardless of treatment, clinicians and patients should select nonpharmacologic treatment with superficial heat (moderate-quality evidence), massage, acupuncture, or spinal manipulation (low-quality evidence). If pharmacologic treatment is desired, clinicians and patients should select nonsteroidal anti-inflammatory drugs or skeletal muscle relaxants (moderate-quality evidence). (Grade: strong recommendation)
- For patients with chronic low back pain, clinicians and patients should initially select nonpharmacologic treatment with exercise, multidisciplinary rehabilitation, acupuncture, mindfulness-based stress reduction (moderate-quality evidence), tai chi, yoga, motor control exercise, progressive relaxation, electromyography biofeedback, low-level laser therapy, operant therapy, cognitive behavioral therapy, or spinal manipulation (low-quality evidence). (Grade: strong recommendation)
- In patients with chronic low back pain who have had an inadequate response to nonpharmacologic therapy, clinicians and patients should consider pharmacologic treatment with nonsteroidal anti-inflammatory drugs as first-line therapy, or tramadol or duloxetine as second-line therapy. Clinicians should only consider opioids as an option in patients who have failed the aforementioned treatments and only if the potential benefits outweigh the risks for individual patients and after a discussion of known risks and realistic benefits with patients. (Grade: weak recommendation, moderate-quality evidence)
Red flags may help identify cases of nonmechanical low backache and prompt further evaluation or imaging which include.
- A progressive motor or sensory loss,
- New urinary retention or overflow incontinence,
- History of cancer,
- A recent invasive spinal procedure,
- Significant trauma relative to age.
Imaging Modalities
- Imaging on initial presentation should be reserved for when there is suspicion for cauda equina syndrome, malignancy, fracture, or infection.
- Plain radiography of the lumbar spine is appropriate to assess for fracture and bony abnormality
- Magnetic resonance imaging is better for identifying the source of neurologic or soft tissue abnormalities. .
Acute/Subacute Low Back Pain
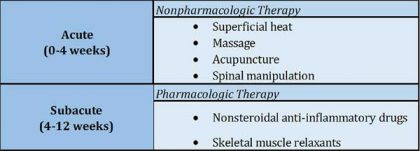
Both nonpharmacologic and pharmacologic therapies are available for the management of acute and subacute low back pain (Table 1).
Nonpharmacologic and Pharmacologic Treatment for the Management of Acute and Subacute Low Back Pain
Nonpharmacologic Therapy
- Current recommendations suggest that clinicians select nonpharmacologic therapies prior to instituting the use of pharmacologic agents.
- Specific nonpharmacologic therapies that have proven efficacious in treating acute and/or subacute low back pain include the use of superficial heat, massage, acupuncture, and spinal manipulation.
Pharmacological Therapy
- Majority of pharmacologic treatment modalities currently used for acute and subacute low back pain have shown little to small effect on patients' pain levels and functional abilities.
- But 2 categories of drugs — nonsteroidal anti-inflammatory drugs (NSAIDs) and skeletal muscle relaxants (SMRs) — have demonstrated evidence for improving the quality of life for patients with acute or subacute low back pain.
Chronic Low Back Pain
Nonpharmacologic and pharmacologic therapies have been identified for the management of chronic low backache (Table 2).
Nonpharmacologic and Pharmacologic Treatment for the Management of Chronic Low Back Pain
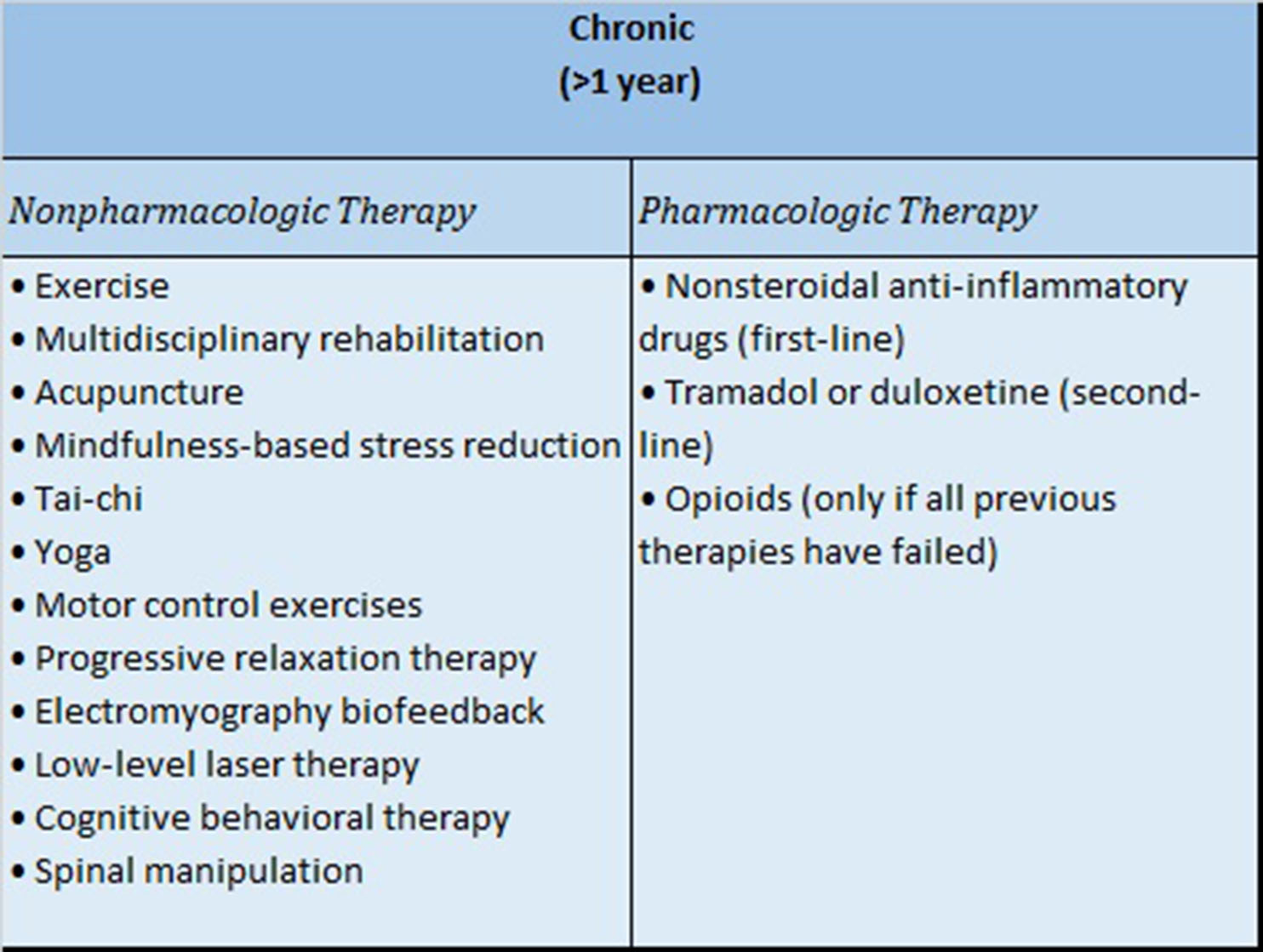
Nonpharmacologic Therapy
- In chronic low backache, the American College of Physicians recommends initial treatment to include nonpharmacologic therapies as the first-line option because they are safe as compared with pharmacologic therapies.
- Several nonpharmacologic therapies for chronic low backache include the use of exercise, acupuncture, and mindfulness-based stress reduction.
- Other nonpharmacologic therapies recommended in the treatment of chronic low backache include tai-chi,yoga, motor control include tai-chi, relaxation therapy, electromyography biofeedback, low-level laser therapy, cognitive behavioral therapy, and spinal manipulation.
Pharmacologic Therapy
- Pharmacologic therapy should only be considered for patients with chronic low backache if there has been an inadequate response to nonpharmacologic management.
- First-line therapy for chronic low back pain should include the use of NSAIDs that have shown efficacy in reducing pain and increasing functional ability.
- Progression to second-line therapy, should the patient not be a candidate for NSAIDs or should treatment with NSAIDs fail, includes consideration of tramadol or duloxetine.
- The use of tramadol or duloxetine has been associated with decreased pain and increased functional ability in patients with chronic low back pain but clinicians should be cautious in light of the risk of abuse associated with tramadol.
- When all nonpharmacologic and nonnarcotic pharmacologic efforts have been exhausted and the patient continues to experience chronic low back pain, the clinician may consider the use of opioids.
- The clinician should discuss known risks as well as expected, realistic benefits of opioid treatment (short-term reduction in pain and increase in functional ability) with the patient prior to making the decision to prescribe this treatment for chronic low back pain.
Low backache has been found to have a significant economic impact, with substantial direct and indirect healthcare costs. Educating patients on prognosis and incorporating psychosocial components of care such as identifying comorbid psychological problems and barriers to treatment are essential components of long-term management.
For further reference log on to :
http://annals.org/aim/fullarticle/2603228/noninvasive-treatments-acute-subacute-chronic-low-back-pain-clinical-practice

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd