- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Non-healing tissue from diabetic foot ulcers reprogrammed as pluripotent stem cells
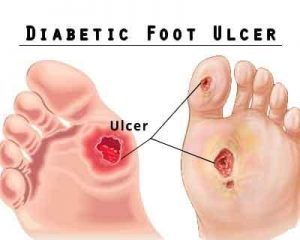
Boston : Researchers at Tufts University School of Dental Medicine and the Sackler School of Graduate Biomedical Sciences at Tufts, led by Jonathan Garlick, have established for the first time that skin cells from diabetic foot ulcers can be reprogrammed to acquire properties of embryonic-like cells. These induced pluripotent stem cells might someday be used to treat chronic wounds. The study is published online in advance of print in Cellular Reprogramming.
A second study from the research team published in Wound Repair and Regeneration found that a protein called fibronectin is linked to a break-down in the wound-healing process in cells from diabetic foot ulcers.
"The results are encouraging. Unlike cells taken from healthy human skin, cells taken from wounds that don't heal like diabetic foot ulcers are difficult to grow and do not restore normal tissue function," said senior author on both studies, Jonathan Garlick, Ph.D., D.D.S., stem cell researcher at Tufts University School of Dental Medicine in Boston. "By pushing these diabetic wound cells back to this earliest, embryonic stage of development, we have "rebooted" them to a new starting point to hopefully make them into specific cell types that can heal wounds in patients suffering from non-healing wounds."
The research team successfully reprogramed cells from diabetic wounds to an embryonic-like state and turned them into cell types that are important for wound healing. Using three independent criteria, they confirmed that the cells had been reprogrammed to a pluripotent state, which means that they can be turned into a variety of different cell types, including those that can stimulate wound repair.
As a next step, the research team created 3D engineered tissues that they had previously found to mimic many features of chronic wounds. They used these 3D tissues to test the properties of cells from diabetic foot ulcers and found that cells from diabetic ulcers get stuck making an immature scaffold made up predominantly of a protein called fibronectin that is likely to prevent proper closure of wounds. Fibronectin has been shown to be abnormal in other diabetic complications, such as kidney disease, but this is the first study that directly connects it to cells taken from diabetic foot ulcers.
"The development of more effective therapies for foot ulcers has been hampered by the lack of realistic wound healing models that closely mimic the function of the extracellular matrix, which is the scaffold critical for wound repair in skin," said Anna Maione, Ph.D., first author on the Wound Repair and Regeneration study who did this work as part of her Ph.D. studies in Cell, Molecular & Developmental Biology at the Sackler School and her post-doctoral work at Tufts University School of Dental Medicine. "This work builds on our paper published in 2015 that showed that cells from diabetic ulcers have fundamental defects which we can simulate using our 3D tissue models grown in the lab. These models will be a great way to test new therapeutics that could improve wound healing and prevent limb amputation which can result when treatments fail."
"The 3D model is critical because it will allow us to take these studies further. Now that we have confirmed that it's possible to reprogram wound cells to a very early stage of development we need to study if they can turn into more mature cell types and then study them in our 3D models to see if they will improve healing of chronic wounds," said Behzad Gerami-Naini, Ph.D., first author on the study in Cellular Reprogramming and an assistant professor at Tufts University School of Dental Medicine.
"The findings advance commonly-held assumptions about how diabetic foot ulcers develop. Most importantly, our ability to reprogram these cells gives us new treatment avenues to pursue. The big question is since we have created induced pluripotent stem cells which we can now make into many cells types important for wound healing will they be better for wound healing than cells originally taken from the non-healing wound?" asked Garlick, who is also a member of the Cell, Molecular & Developmental Biology program faculty at the Sackler School.
More than 29 million Americans have diabetes. Diabetic foot ulcers, often resistant to treatment, are a major complication. The National Diabetes Statistics Report of 2014 stated that about 73,000 non-traumatic lower-limb amputations in 2010 were performed in adults aged 20 years or older with diagnosed diabetes, and approximately 60 percent of all non-traumatic lower-limb amputations occur in people with diabetes.
Garlick's lab at Tufts Dental School performs research at the intersection of tissue engineering and stem cell biology. Dr. Garlick and his colleagues work to grow tissues that mimic diabetic wounds from induced pluripotent stem cells by reprogramming adult cells to grown skin that mimics a range of skin diseases, including cancer and scleroderma. Their goal is to develop experimental approaches for precision therapies that may regenerate and repair diseased or damaged tissues and organs.
Additional authors on the study in Cellular Reprogramming are Avi Smith, Anna G. Maione, Olga Kashpur, and Gianpaolo Carpinito, all of Tufts University School of Dental Medicine; Aristides Veves of Beth Israel Deaconess Medical Center; and David J. Mooney of Harvard University and the Wyss Institute for Biologically Inspired Engineering.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd