- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
NICE Guidelines on acute Prostatitis
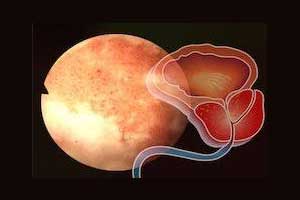
NICE has released ts latest guidelines on acute Prostatitis.
Following are the major recommendations for managing acute prostatitis:
1)Be aware that acute prostatitis:
- is a bacterial infection of the prostate needing treatment with antibiotics,
- is usually caused by bacteria entering the prostate from the urinary tract,
- can occur spontaneously or after medical procedures such as a prostate biopsy,
- can last several weeks and
- can cause complications such as acute urinary retention and prostatic abscess.
A) Offer an antibiotic to people with acute prostatitis. Take account of:
- the severity of symptoms
- the risk of developing complications or having treatment failure, particularly after medical procedures such as prostate biopsy
- previous urine culture and susceptibility results
- previous antibiotic use, which may have led to resistant bacteria.
B) Obtain a midstream urine sample before antibiotics are taken and send for culture and susceptibility testing.
C) When results of urine cultures are available:
- review the choice of antibiotic, and
- change the antibiotic according to susceptibility results if the bacteria are resistant, using a narrow spectrum antibiotic wherever possible.
D) Advice when an antibiotic prescription is given
a)When an antibiotic is given, give advice about:
- the usual course of acute prostatitis (several weeks)
- possible adverse effects of the antibiotic, particularly diarrhea and nausea
- seeking medical help if:
- symptoms worsen at any time, or
- symptoms do not start to improve within 48 hours of taking the antibiotic, or
- the person becomes systemically very unwell.
E) Reassessment
a)Reassess if symptoms worsen at any time, taking account of:
- other possible diagnoses
- any symptoms or signs suggesting a more serious illness or condition, such as acute urinary retention, prostatic abscess or sepsis
- previous antibiotic use, which may have led to resistant bacteria.
F) Referral
a)Refer people with acute prostatitis to the hospital if:
- they have any symptoms or signs suggesting a more serious illness or condition (for example sepsis, acute urinary retention or prostatic abscess), or
- their symptoms are not improving 48 hours after starting the antibiotic.
3.Self-care
- Advise people with acute prostatitis about using paracetamol (with or without a low‑dose weak opioid, such as codeine) for pain, or ibuprofen if this is preferred and suitable.
- Advise people with acute prostatitis about drinking enough fluids to avoid dehydration.
4.Choice of antibiotic
- When prescribing an antibiotic for acute prostatitis, take account of local antimicrobial resistance data and follow table 1 for adults aged 18 years and over
- Give oral antibiotics first line if the person can take oral medicines, and the severity of their condition does not require intravenous antibiotics.
- Review intravenous antibiotics by 48 hours and consider stepping down to oral antibiotics where possible.
- Review antibiotic treatment after 14 days and either stop the antibiotic or continue for a further 14 days if needed, based on an assessment of the person's history, symptoms, clinical examination, urine and blood tests.
Table 1 Antibiotics for adults aged 18 years and over
| Antibiotic | Dosage and course length |
| First-choice oral antibiotic (guided by susceptibilities when available) | |
| Ciprofloxacin | 500 mg twice a day for 14 days then review |
| Ofloxacin | 200 mg twice a day for 14 days then review |
| Alternative first-choice oral antibiotic for adults unable to take a fluoroquinolone (guided by susceptibilities when available) | |
| Trimethoprim | 200 mg twice a day for 14 days then review |
| Second-choice oral antibiotic (after discussion with specialist) | |
| Levofloxacin | 500 mg once a day for 14 days then review |
| Co‑trimoxazole | 960 mg twice day for 14 days then review |
| First-choice intravenous antibiotics (if unable to take oral antibiotics or severely unwell; guided by susceptibilities when available). Antibiotics may be combined if sepsis a concern | |
| Ciprofloxacin | 400 mg twice or three times a day |
| Levofloxacin | 500 mg once a day |
| Cefuroxime | 1.5 g three or four times a day |
| Ceftriaxone | 2 g once a day |
| Gentamicin | Initially 5 to 7 mg/kg once a day, subsequent doses adjusted according to serum gentamicin concentration |
| Amikacin | Initially 15 mg/kg once a day (maximum per dose 1.5 g once a day), subsequent doses adjusted according to serum amikacin concentration (maximum 15 g per course) |
| Second-choice intravenous antibiotic | |
| Consult local microbiologist | |
| 1 See BNF for appropriate use and dosing in specific populations, for example, hepatic impairment and renal impairment, and administering intravenous antibiotics. 2 Check any previous urine culture and susceptibility results and antibiotic prescribing and choose antibiotics accordingly. 3 The European Medicines Agency's Pharmacovigilance Risk Assessment Committee has recommended restricting the use of fluoroquinolone antibiotics following a review of disabling and potentially long-lasting side effects mainly involving muscles, tendons, bones and the nervous system (press release October 2018), but they are appropriate in acute prostatitis which is a severe infection. 4 Review treatment after 14 days and either stop the antibiotic or continue for a further 14 days if needed based on clinical assessment. 5 Co-trimoxazole should only be considered when there is bacteriological evidence of sensitivity and good reasons to prefer this combination to a single antibiotic (BNF, August 2018). 6 Review intravenous antibiotics by 48 hours and consider stepping down to oral antibiotics where possible for a total of 14 days then review. 7 Therapeutic drug monitoring and assessment of renal function is required (BNF, August 2018). | |
To Read the Complete Guidelines, Click on the following link: https://www.nice.org.uk/guidance/ng110

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd