- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
NICE 2019 Guidelines for management of Crohn’s disease
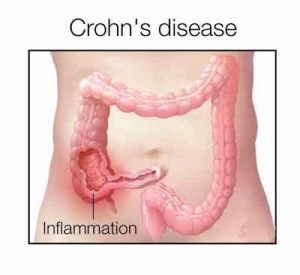
NICE has released its 2019 guidelines on the management of Crohn’s disease. This guideline covers the management of Crohn’s disease in children, young people and adults. It aims to reduce people’s symptoms and maintain or improve their quality of life.
Crohn's disease is an idiopathic inflammatory disorder of unknown etiology with genetic, immunologic, and environmental influences. The incidence of Crohn's disease has steadily increased over the past several decades.
Following are the major recommendations:
1. Providing information and support
- Ensure that information and advice about Crohn's disease:
- is age appropriate
- is of the appropriate cognitive and literacy level
- meets the cultural and linguistic needs of the local community. [2012]
- Discuss treatment options and monitoring with the person with Crohn's disease, with their family members or carers (as appropriate), and within the multidisciplinary team. Apply the principles in the NICE guideline on patient experience in adult NHS services. [2012]
- Discuss the possible nature, frequency and severity of side effects of drug treatment with people with Crohn's disease and their family members or carers (as appropriate). [2012]
- Give all people with Crohn's disease and their family members or carers (as appropriate) information, advice and support in line with published NICE guidance on:
- smoking cessation
- patient experience
- medicines adherence
- fertility. [2012]
- Give people with Crohn's disease and their family members or carers additional information on the following when appropriate:
- possible delay of growth and puberty in children and young people
- diet and nutrition
- fertility and sexual relationships
- prognosis
- side effects of their treatment
- cancer risk
- surgery
- transition between paediatric and adult services
- contact details for support groups. [2012]
- Offer people with Crohn's disease and their family members or carers (as appropriate) age‑appropriate multidisciplinary support to deal with any concerns about the disease and its treatment, including concerns about body image, living with a chronic illness, and attending school and higher education. [2012]
2. Inducing remission in Crohn's disease
Monotherapy
- Offer monotherapy with a conventional glucocorticosteroid (prednisolone, methylprednisolone or intravenous hydrocortisone) to induce remission in people with a first presentation or a single inflammatory exacerbation of Crohn's disease in a 12‑month period. [2012]
- Consider enteral nutrition as an alternative to a conventional glucocorticosteroid to induce remission for:
- children in whom there is concern about growth or side effects and
- young people in whom there is concern about growth. [2012]
- Consider budesonide for a first presentation or a single inflammatory exacerbation in a 12‑month period for people:
- who have one or more of distal ileal, ileocaecal or right-sided colonic disease and
- if conventional glucocorticosteroids are contraindicated, or if the person declines or cannot tolerate them.Explain that budesonide is less effective than a conventional glucocorticosteroid, but may have fewer side effects. [2012]
- Consider aminosalicylate treatment for a first presentation or a single inflammatory exacerbation in a 12‑month period if conventional glucocorticosteroids are contraindicated, or if the person declines or cannot tolerate them. Explain that aminosalicylates are less effective than a conventional glucocorticosteroid or budesonide but may have fewer side effects than a conventional glucocorticosteroid. [2012]
- Do not offer budesonide or aminosalicylate treatment for severe presentations or exacerbations. [2012]
- Do not offer azathioprine, mercaptopurine or methotrexate as monotherapy to induce remission. [2012]
Add‑on treatment
- Consider adding azathioprine or mercaptopurine to a conventional glucocorticosteroid or budesonide to induce remission of Crohn's disease if:
- there are 2 or more inflammatory exacerbations in a 12‑month period or
- the glucocorticosteroid dose cannot be tapered. [2012]
- Assess thiopurine methyltransferase (TPMT) activity before offering azathioprine or mercaptopurine. Do not offer azathioprine or mercaptopurine if TPMT activity is deficient (very low or absent). Consider azathioprine or mercaptopurine at a lower dose if TPMT activity is below normal but not deficient (according to local laboratory reference values). [2012]
- Consider adding methotrexate to a conventional glucocorticosteroid or budesonide to induce remission in people who cannot tolerate azathioprine or mercaptopurine, or in whom TPMT activity is deficient, if:
- there are 2 or more inflammatory exacerbations in a 12‑month period or
- the glucocorticosteroid dose cannot be tapered. [2012]
- Monitor the effects of azathioprine, mercaptopurine and methotrexate as advised in the British national formulary (BNF) or British national formulary for children (BNFC). Monitor for neutropenia in people taking azathioprine or mercaptopurine even if they have normal TPMT activity. [2012]
- Ensure that there are documented local safety monitoring policies and procedures (including audit) for people receiving treatment that needs monitoring. Nominate a member of staff to act on abnormal results and communicate with GPs, people with Crohn's disease and their family members or carers (as appropriate). [2012]
Infliximab and adalimumab
- Infliximab and adalimumab, within their licensed indications, are recommended as treatment options for adults with severe active Crohn's disease whose disease has not responded to conventional therapy (including immunosuppressive and/or corticosteroid treatments), or who are intolerant of or have contraindications to conventional therapy. Infliximab or adalimumab should be given as a planned course of treatment until treatment failure (including the need for surgery), or until 12 months after the start of treatment, whichever is shorter. People should then have their disease reassessed to determine whether ongoing treatment is still clinically appropriate. [2010]
- Treatment should normally be started with the less expensive drug (taking into account drug administration costs, required dose and product price per dose). This may need to be varied for individuals because of differences in the method of administration and treatment schedules. [2010]
- When a person with Crohn's disease is starting infliximab or adalimumab discuss options of:
- monotherapy with one of these drugs or
- combined therapy (either infliximab or adalimumab, combined with an immunosuppressant).Tell the person there is uncertainty about the comparative effectiveness and long‑term adverse effects of monotherapy and combined therapy. [2016]
- Infliximab, within its licensed indication, is recommended as a treatment option for people with active fistulising Crohn's disease whose disease has not responded to conventional therapy (including antibiotics, drainage and immunosuppressive treatments), or who are intolerant of or have contraindications to conventional therapy. Infliximab should be given as a planned course of treatment until treatment failure (including the need for surgery) or until 12 months after the start of treatment, whichever is shorter. People should then have their disease reassessed to determine whether ongoing treatment is still clinically appropriate. [2010]
- Treatment with infliximab or adalimumab should only be continued if there is clear evidence of ongoing active disease as determined by clinical symptoms, biological markers and investigation, including endoscopy if necessary. Specialists should discuss the risks and benefits of continued treatment with patients and consider a trial withdrawal from treatment for all patients who are in stable clinical remission. People who continue treatment with infliximab or adalimumab should have their disease reassessed at least every 12 months to determine whether ongoing treatment is still clinically appropriate. People whose disease relapses after treatment is stopped should have the option to start treatment again. [2010]
- Infliximab, within its licensed indication, is recommended for the treatment of people aged 6 to 17 years with severe active Crohn's disease whose disease has not responded to conventional therapy (including corticosteroids, immunomodulators and primary nutrition therapy), or who are intolerant of or have contraindications to conventional therapy. The need to continue treatment should be reviewed at least every 12 months. [2010]
- For the purposes of this guidance, severe active Crohn's disease is defined as very poor general health and one or more symptoms such as weight loss, fever, severe abdominal pain and usually frequent (3 to 4 or more) diarrhoeal stools daily. People with severe active Crohn's disease may or may not develop new fistulae or have extra‑intestinal manifestations of the disease. This clinical definition normally, but not exclusively, corresponds to a Crohn's Disease Activity Index (CDAI) score of 300 or more, or a Harvey‑Bradshaw score of 8 to 9 or above. [2010]
- When using the CDAI and Harvey‑Bradshaw Index, healthcare professionals should take into account any physical, sensory or learning disabilities, or communication difficulties that could affect the scores and make any adjustments they consider appropriate. [2010]
- Treatment with infliximab or adalimumab should only be started and reviewed by clinicians with experience of TNF inhibitors and of managing Crohn's disease. [2010]
Ustekinumab and vedolizumab
- For guidance on using ustekinumab, see the NICE technology appraisal guidance on ustekinumab for moderately to severely active Crohn's disease after previous treatment. [2019]
- For guidance on using vedolizumab, see the NICE technology appraisal guidance on vedolizumab for treating moderately to severely active Crohn's disease after prior therapy. [2019]
3. Maintaining remission in Crohn's disease
- Discuss with people with Crohn's disease and their family members or carers (as appropriate) options for managing their disease when they are in remission, including both no treatment and treatment. The discussion should include the risk of inflammatory exacerbations (with and without drug treatment) and the potential side effects of drug treatment. Record the person's views in their notes. [2012]
- Offer colonoscopic surveillance in line with the NICE guideline on colorectal cancer prevention: colonoscopic surveillance in adults with ulcerative colitis, Crohn's disease or adenomas. [2012]
Follow‑up during remission for people who choose not to have a maintenance treatment
- When people choose not to receive maintenance treatment:
- discuss and agree with them and their family members or carers (as appropriate) plans for follow‑up, including the frequency of follow‑up and who they should see
- ensure they know which symptoms may suggest a relapse and should prompt a consultation with their healthcare professional (most frequently, unintended weight loss, abdominal pain, diarrhoea, general ill‑health)
- ensure they know how to access the healthcare system if they experience a relapse
- discuss the importance of not smoking. [2012]
Maintenance treatment for people who choose this option
- Offer azathioprine or mercaptopurine as monotherapy to maintain remission when previously used with a conventional glucocorticosteroid or budesonide to induce remission. [2012]
- Consider azathioprine or mercaptopurine to maintain remission in people who have not previously received these drugs (particularly people with adverse prognostic factors such as early age of onset, perianal disease, glucocorticosteroid use at presentation and severe presentations). [2012]
- Consider methotrexate to maintain remission only in people who:
- needed methotrexate to induce remission or
- have tried but did not tolerate azathioprine or mercaptopurine for maintenance or
- have contraindications to azathioprine or mercaptopurine (for example, deficient thiopurine methyltransferase [TPMT] activity or previous episodes of pancreatitis). [2012]
- Do not offer a conventional glucocorticosteroid or budesonide to maintain remission. [2012]
4. Maintaining remission in Crohn's disease after surgery
- To maintain remission in people with ileocolonic Crohn's disease who have had complete macroscopic resection within the last 3 months, consider azathioprine in combination with up to 3 months' postoperative metronidazole. [2019]
- Consider azathioprine alone for people who cannot tolerate metronidazole. [2019]
- Monitor the effects of azathioprine and metronidazole as advised in the British national formulary(BNF) or British national formulary for children (BNFC). Monitor for neutropenia in people taking azathioprine even if they have normal thiopurine methyltransferase (TPMT) activity. [2019]
- Do not offer biologics to maintain remission after complete macroscopic resection of ileocolonic Crohn's disease. [2019]
- For people who have had surgery and started taking biologics before this guideline was published (May 2019), continue with their current treatment until both they and their NHS healthcare professional agree it is appropriate to change. [2019]
- Do not offer budesonide to maintain remission in people with ileocolonic Crohn's disease who have had complete macroscopic resection. [2019]
5. Surgery
Crohn's disease limited to the distal ileum
- Consider surgery as an alternative to medical treatment early in the course of the disease for people whose disease is limited to the distal ileum, taking into account the following:
- benefits and risks of medical treatment and surgery
- risk of recurrence after surgery
- individual preferences and any personal or cultural considerations.Record the person's views in their notes. [2012]
- Consider surgery early in the course of the disease, or before or early in puberty, for children and young people whose disease is limited to the distal ileum and who have:
- growth impairment despite optimal medical treatment and/or
- refractory disease.Discuss treatment options with the child or young person and their family members or carers (as appropriate), and within the multidisciplinary team. [2012]
Managing strictures
- Consider balloon dilation, particularly for people with a single stricture that is short, straight and accessible by colonoscopy. [2012]
- Discuss the benefits and risks of balloon dilation and surgical interventions for managing structures with:
- the person with Crohn's disease and their family members or carers (as appropriate) and
- a surgeon and
- a gastroenterologist. [2012]
- Take into account the following factors when assessing options for managing a stricture:
- whether medical treatment has been optimised
- the number and extent of previous resections
- the rapidity of past recurrence (if appropriate)
- the potential for further resections
- the consequence of short bowel syndrome
- the person's preference, and how their lifestyle and cultural background might affect management. [2012]
- Ensure that abdominal surgery is available for managing complications or failure of balloon dilation. [2012]
6. Monitoring for osteopenia and assessing fracture risk
Refer to the NICE guideline on osteoporosis: assessing the risk of fragility fracture for recommendations on assessing the risk of fragility fracture in adults. Crohn's disease is a cause of secondary osteoporosis.
- Do not routinely monitor for changes in bone mineral density in children and young people. [2012]
- Consider monitoring for changes in bone mineral density in children and young people with risk factors, such as low body mass index (BMI), low trauma fracture or continued or repeated glucocorticosteroid use. [2012]
7. Conception and pregnancy
- Give information about the possible effects of Crohn's disease on pregnancy, including the potential risks and benefits of medical treatment and the possible effects of Crohn's disease on fertility. [2012]
- Ensure effective communication and information‑sharing across specialties (for example, primary care, obstetrics and gastroenterology) in the care of pregnant women with Crohn's disease. [2012]
For more details click on the link: www.nice.org.uk

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd