- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
New-onset AF during TAVR increases risk of bleeding and stroke: JACC
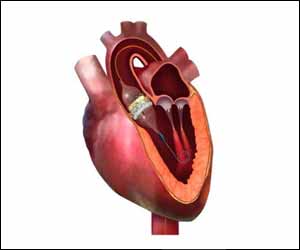
USA: New-onset atrial fibrillation (AF) in patients undergoing transcatheter aortic valve replacement (TAVR) is associated with worse outcomes compared to patients having pre-existing AF or no AF, finds a recent study published in the JACC: Cardiovascular Interventions journal. Worse outcomes included increased risk of mortality and bleeding, stroke, and heart failure hospitalizations.According to Mayo Clinic, atrial fibrillation is an irregular and often rapid heart rate that can increase the risk of strokes, heart failure and other heart-related complications.
Amgad Mentias, University of Iowa Carver College of Medicine, Iowa City, and colleagues evaluated the impact of new-onset and pre-existing AF on TAVR long-term outcomes compared with patients without AF.
The study involved 72,660 patients ≥65 years of age who underwent nonapical TAVR between 2014 and 2016 using Medicare inpatient claims.
History of AF was defined by diagnoses on claims during the 3 years preceding the TAVR, and new-onset AF was defined as the occurrence of AF during the TAVR admission or within 30 days after TAVR in a patient without prior history of AF.
Outcomes included all-cause mortality, and readmission for bleeding, stroke, and heart failure (HF).
Key findings of the study include:
- Overall, 40.7% had pre-existing AF (n = 29,563) and 6.8% experienced new onset AF (n = 2,948) after TAVR.
- Mean age was 81.3, 82.4, and 83.8 years in patients with no AF, pre-existing, and new-onset AF, respectively.
- Pre-existing AF patients had the highest burden of comorbidities.
- After a follow-up of 73,732 person-years, mortality was higher with new-onset AF compared with pre-existing and no AF (29.7, 22.6, and 12.8 per 100 person-years, respectively).
- After adjusting for patient characteristics and hospital TAVR volume, new-onset AF remained associated with higher mortality compared with no AF (adjusted hazard ratio: 2.068) and pre-existing AF (adjusted hazard ratio: 1.35).
- In competing risk analysis, new-onset AF was associated with a higher risk of bleeding (subdistribution hazard ratio [sHR]: 1.66), stroke (sHR: 1.92), and HF (sHR: 1.98) compared with pre-existing AF.
"In patients undergoing TAVR, new-onset AF is associated with increased risk of mortality and bleeding, stroke, and HF hospitalizations compared with pre-existing AF or no AF," concluded the authors.
More Information: "Impact of Pre-Existing and New Onset Atrial Fibrillation on Outcomes After Transcatheter Aortic Valve Replacement" published in JACC: Cardiovascular Interventions journal.
DOI: 10.1016/j.jcin.2019.06.019
Journal Information: JACC: Cardiovascular Interventions

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd