- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
New nerve stimulation therapy effective for refractory back pain
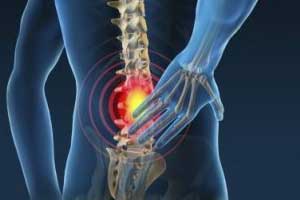
Dorsal root ganglion stimulation could provide long-term relief for chronic back pain that was unresponsive to other treatments, including spinal cord stimulation. This is helpful to those needing a non-drug form of pain therapy also.
The study was presented at the 2018 annual meeting of the American Society of Anesthesiologists in San Francisco, CA.
Robert J. McCarthy, a professor of anesthesiology at Rush Medical College, and colleagues conducted the study to evaluate pain and disability in patients with chronic pain who underwent permanent DRG stimulator placement for chronic lower extremity and back pain.
"Those who received the DRG stimulation had tried numerous therapies, from drugs to spinal cord stimulation to surgery, but got little to no lasting pain relief," says McCarthy.
They reported "significant improvement in pain even after a year, which is notable," he suggests, adding that, "For most, DRG stimulation really improved their quality of life."
Although it often accompanies many persistent medical conditions, scientists increasingly believe that chronic pain is a "health concern on its own."
Chronic pain is pain that continues for at least 3 months. It arises when the pain signals that travel to the brain along nerve fibers persist, even though the source of the pain has disappeared.
The researchers investigated the effectiveness of DRG stimulation in 67 people with chronic back pain by following them for 3-18 months after implantation. Of these, 17 had the implant for at least 12 months.
People self-assessed their levels of pain on a scale of 1–10 — with 10 representing "the worst pain imaginable" — both before implantation and during follow-up meetings.
Also Read: Noninvasive Treatments of low back pain: ACP Guideline
Key Findings:
- Before receiving their DRG implant, most of those in the study rated their pain at level 8. Afterward, the most common pain score was 5, which represents a drop of 33 percent. The researchers describe the improvement as "clinically significant."
- There was also a similar decrease in self-reported disability, with a median drop of 27 percent. Researchers defined disability as "limitations in daily living" caused by pain.
- When asked if the treatment was helpful, 94 percent of those receiving it said yes.
- One person had to have the DRG stimulator removed because of a complication, two people had to have their devices removed following infection, and five others had to have the wires re-inserted.
Prof. McCarthy notes that the DRG stimulator device is not an easy option because of the difficulty involved in placing the electrodes accurately. It could be an alternative, however, for those people who have not experienced any benefit from other treatments.
It could also "reduce or eliminate the need for opioids," he concludes.
Spinal cord and DRG stimulation
Spinal cord stimulation treatment involves implantation of a small device that sends low-voltage electrical impulses along a wire placed along the spinal cord. The effect is to block pain signals from reaching the brain.
Dorsal root ganglia are clusters of nerve cells — located on each side of the spinal vertebra — that relay pain and sensory signals coming from various parts of the body to the spinal cord and brain.
DRG stimulation disrupts the signals by delivering small electrical pulses through a wire placed alongside the specific DRG associated with the source of the pain. This replaces extreme pain with a more bearable sensation, such as numbness or tingling.
The DRG stimulation works by targeting only the nerve fibers carrying signals from the source of pain. Unlike spinal cord stimulation, it avoids nerve fibers that convey messages from non-painful regions.
Scientists implant the device, which looks like a small pacemaker, in the lower back under the skin. A pain specialist sets the amount of current that it delivers according to the amount of pain a person experiences.
The idea of DRG stimulation is attractive because, unlike spinal cord stimulation, it only targets the affected nerves. Another reason is that it requires lower levels of electrical current since less spinal fluid covers the targeted DRG than covers the spinal cord.
For further reference follow the link: http://asaabstracts.com/strands/asaabstracts/abstract.htm?year=2018&index=3&absnum=4403

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd