- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
New Meal-detection technology administers insulin automatically with accuracy
Researchers at Stevens Institute of have developed a system that can detect when a person is eating and calculate how many carbohydrates they are consuming with unprecedented accuracy and speed.This may allow release of insulin for administration closer to the time when it's actually needed, reducing dangerous swings in blood sugar levels.
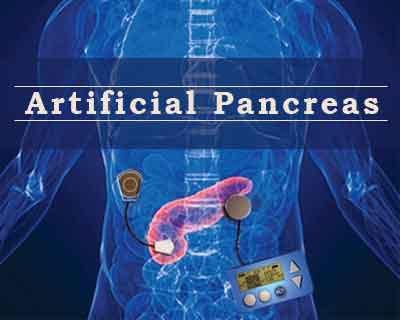
The new meal-detection technology has brought 'artificial pancreas' one step closer to reality.The research has appeared in the Journal of the American Medical Informatics Association.
The work provides a significant advance for people who wear continuous glucose monitors as part of their diabetes treatment, allowing insulin to be administered closer to the time when it's actually needed, reducing dangerous swings in blood glucose levels.
The new system estimates carbohydrate intake accurately and quickly and adjust insulin dosage - sometimes while a person is still eating - allowing insulin to be administered closer to the time when it's actually needed. On average, the system can detect meals within 25 minutes - much faster than the 48 minutes needed by the best previous systems.
The diabetes epidemic is on and by 2050 629 million people likely to be diagnosed with diabetes.In last two decades continuous glucose monitoring, or CGM, systems and insulin pumps have revolutionized at-home care for millions of people with diabetes, reducing the need for painful pinprick tests and manual insulin injections. However, this process is still cumbersome. People with diabetes must input the number of carbohydrates to be eaten; the CGM detects changes in glucose levels; then patients manage the insulin dose to counterbalance carbohydrates in the meal - usually 1 unit of insulin for every 15 grams of carbohydrates to be eaten, although this varies by patient depending on insulin sensitivity.
"This brings us a step closer to the holy grail -- an 'artificial pancreas' that can quickly detect glucose changes, and correct them with an insulin pump, without the user having to do anything," said Samantha Kleinberg, a wearable technologies expert and computer scientist at Stevens.
Announcing a meal is a significant burden as it must be done for every single meal and snack, and can lead to insulin dosing administered incorrectly. Past meal-detection systems have also focused on predicting changes in glucose levels, but Kleinberg and her team, including Min Zhen and Baohua Ni, took a different approach.
Instead of forecasting glucose variations directly, their meal-detection system compares variances in CGMs and physical activity data with the kinds of variances that would be expected from a range of different meals. "We're simulating all the different kinds of meals a person could be eating, and using those simulations to explain the data coming in from the sensors," explained Kleinberg.
The system's estimates about a person's meals are remarkably accurate: carbohydrate intake can be modeled accurately to within 1.2 grams, versus an average error rate of more than 17 grams in the best previous systems.
The new system estimates carbohydrate intake accurately and quickly and adjust insulin dosage - sometimes while a person is still eating - allowing insulin to be administered closer to the time when it's actually needed. On average, the system can detect meals within 25 minutes - much faster than the 48 minutes needed by the best previous systems.
By incorporating activity data, the Stevens system can also account for fluctuations in blood sugar levels caused by exercise, further boosting its accuracy. Future versions could be refined still further by incorporating data from menstrual tracking apps, sleep tracking tools, or physiological stress markers.
For now, though, the focus is on using bigger data sets to develop more accurate simulations. The published results were based on three days of data for each participant. Kleinberg is now working to develop algorithms that improve over time, growing faster and more accurate as they learn about their user's dietary habits and physiological responses.
The system could also monitor the effects of different insulin doses, notifying users when they miss a dose or helping to fine-tune dosage levels. "Missed insulin with meals is a major problem," Kleinberg said. "If we can detect the size of a meal, we can offer suggestions about how much insulin is needed in response."
For further reference log on to:
http://dx.doi.org/10.1093/jamia/ocz159
Journal-Journal of the American Medical Informatics Association
artificial pancreasautomaticallyblood sugarFastinsulin administrationJournal of the American Medical Informatics AssociationMeal-detection technology
Source : Journal of the American Medical Informatics AssociationNext Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd