- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
New guideline on pelvic girdle pain during pregnancy
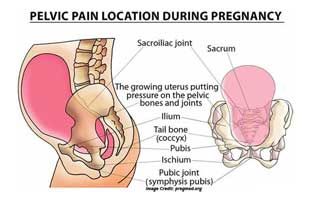
Pelvic girdle pain (PGP) is a common condition that causes pain and physical impairment, most frequently during the antepartum (before delivery) period. A new guideline for evidence-based physical therapy practice for PGP during pregnancy appears in the Journal of Women's Health Physical Therapy, official (SOWH) of the American Physical Therapy Association. The journal is published by Wolters Kluwer.
Created by the authors for the SOWH and Orthopedic Section of the APTA, the new document presents a clinical practice guideline for physical therapy management for PGP in the antepartum population. The lead author is Susan C. Clinton, PT, DScPT, COMT, OCS, WCS, FAAOMPT, of Embody Physiotherapy & Wellness, LLC, Sewickley, Pa.
Antepartum Pelvic Girdle Pain - Guideline for Physical Therapy Management
Pelvic girdle pain is estimated to occur in up to 70 percent of women sometime during pregnancy. Women with PGP develop pain in the pelvic region, which sometimes brings changes in posture, gait, and activity level. These symptoms can cause significant impairment in several areas of patients' lives.
Symptoms of PGP may be severe in 20 percent of women, and in some cases may persist after delivery. Physical therapists play an important role in assessment and management of women with patients with PGP during and after pregnancy.
The new guideline makes recommendations for physical therapy management in key areas. Recommendations are ranked by strength of supporting evidence and address specific categories of impairment based on body function, body structure, and activities/participation. Topics include:
- Risk factors. Based on strong evidence, risk factors for the development of or more severe PGP include previous pregnancy, orthopedic dysfunction (such as hip and/or leg dysfunction), increased body mass index, and smoking. Risk is also higher for patients with work dissatisfaction and those who don't believe that their condition will improve.
- Clinical course. Several factors can help to identify women who will have persistent problems. These include PGP developing early in pregnancy, multiple pain locations, and abnormal results on multiple physical therapy assessments.
- Examination and diagnosis. The guideline highlights the importance of recognizing other pregnancy-related conditions that may appear similar to PGP. Important clinical tests and outcome questionnaires for assessing women with PGP are identified as well.
- Physical therapy interventions. Physical therapy recommendations for PGP may include the use of a support belt, exercise programs, or manual therapy techniques. Yet so far there is only weak or conflicting evidence to support these recommendations. While strong evidence shows that women with PGP are at high risk of falls, there is little evidence on measures to assess balance or reduce the risk of falls, including activity limitations.
The new document is part of the SOWH's ongoing effort to create evidence-based practice guidelines for women's health and orthopedic physical management of patients with musculoskeletal impairments described in the World Health Organization's International Classification of Functioning, Disability, and Health (ICF). The full guideline is available on the Journal of Women's Health Physical Therapy and the Section on Women's Health websites.
The authors believe their research review and evidence-based guideline will provide a useful guide to diagnosis, management, and outcomes assessment for the common problem of PGP, with interventions guided by the individual patient's physical impairment. Susan Clinton adds, "The creation of this guideline also has a very important role in informing research where evidence is sparse in the literature."

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd