- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
New AGA guideline for treatment of mild-to-moderate ulcerative colitis
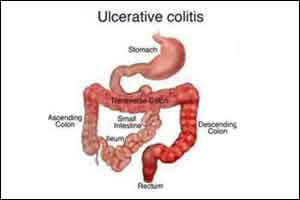
American Gastroenterological Association (AGA) has released new clinical guideline on treatment of mild-to-moderate ulcerative colitis. The new clinical guideline addresses the medical management of these patients, focusing on the use of both oral and topical 5-aminosalicylates (5-ASA) medications, rectal corticosteroids and oral budesonide, to promote high-quality care for UC patients. It has been published in Gastroenterology, the official journal of AGA.
AGA's new clinical guideline is meant to help with the management of patients with mild-to-moderate UC, but not all patients will effectively respond to the outlined therapies. In those cases, there may be a need to escalate treatment to systemic corticosteroids, immunomodulators and/or biologic therapies for induction and maintenance of remission. However, the use of biologic therapies and/or immunomodulators are not specifically addressed within the guideline.
Mild-to-moderate UC was defined as patients with fewer than four to six bowel movements per day, mild or moderate rectal bleeding, the absence of constitutional symptoms, low overall inflammatory burden, and absence of features suggestive of high inflammatory activity. Although disease activity exists on a spectrum, patients in the mild-to-moderate category who have more frequent bowel movements, more prominent rectal bleeding or greater overall inflammatory burden should be considered to have a moderate disease.
The guideline recommends the following for the medical management of mild-to-moderate UC:
- Use either standard dose mesalamine (2-3 grams/day) or diazo-bonded 5-ASA rather than low dose mesalamine, sulfasalazine or no treatment in patients with extensive mild-moderate UC. (Strong recommendation, moderate quality evidence)
- In patients with extensive or left-sided mild-moderate UC, add rectal mesalamine to oral 5-ASA. (Conditional recommendation, moderate quality evidence)
- In patients with mild-moderate UC with suboptimal response to standard-dose mesalamine or diazo-bonded 5-ASA or with moderate disease activity, use high-dose mesalamine (>3 g/d) with rectal mesalamine. (Conditional recommendation, moderate-quality evidence [induction of remission], low-quality evidence [maintenance of remission])
- In patients with mild-moderate UC being treated with oral mesalamine, use once-daily dosing rather than multiple times per day dosing. (Conditional recommendation, moderate quality evidence)
- In patients with mild-moderate UC, use standard-dose oral mesalamine or diazo-bonded 5-ASA, rather than budesonide MMX or controlled ileal-release budesonide for induction of remission. (Conditional recommendation, low quality of evidence)
- In patients with mild-moderate ulcerative proctosigmoiditis or proctitis, use mesalamine enemas (or suppositories) rather than oral mesalamine. (Conditional recommendation, very-low-quality evidence)
- In patients with mild-moderate ulcerative proctosigmoiditis who choose rectal therapy over oral therapy, use mesalamine enemas rather than rectal corticosteroids. (Conditional recommendation, moderate-quality evidence)
- In patients with mild-moderate ulcerative proctitis who choose rectal therapy over oral therapy, use mesalamine suppositories. (Strong recommendation, moderate-quality evidence)
- In patients with mild-moderate ulcerative proctosigmoiditis or proctitis being treated with rectal therapy who are intolerant of or refractory to mesalamine suppositories, use rectal corticosteroid therapy rather than no therapy for induction of remission. (Conditional recommendation, low-quality evidence)
- In patients with mild-moderate UC refractory to optimized oral and rectal 5-ASA, regardless of disease extent, add either oral prednisone or budesonide MMX. (Conditional recommendation, low-quality evidence)
- In patients with mild-moderate UC , AGA makes no recommendation for use of probiotics. (No recommendation, knowledge gap)
- In patients with mild-moderate UC despite 5-ASA therapy, AGA makes no recommendation for use of curcumin. (No recommendation, knowledge gap)
- In patients with mild-moderate UC without Clostridium difficile infection, AGA recommends fecal microbiota transplantation be performed only in the context of a clinical trial. (No recommendation for treatment of ulcerative colitis, knowledge gap)
Ulcerative colitis (UC) is an inflammatory bowel disease (IBD) that is most frequently seen in young adults. It is a chronic illness, of which the severity is classified as mild-to-moderate or moderate-to-severe. Most patients experience mild-to-moderate symptoms, with periods of remission and relapse. About 15 to 30 percent of patients with IBD have a family member with the disease. There is research underway to find out if a certain gene or a group of genes makes a person more likely to have IBD.

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd