- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Multi Modality Approach in Managing Triple Vessel Disease-Case by Dr Sridhar Kasturi
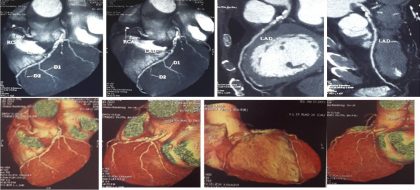
68 yrs old male presented with chest pain associated with shortness of breath. On Examination-PR-84/min, Bp-120/70mmHg, CVS-Heart-S1+,S2+,S30,S40, Lungs-clear,Investigations-Hb-12.0g%, Serum Creatinine-1.0mg/dl ,Blood urea-24mg/dl, RBS-125mg/dl, HIV,HBSAG,HCV-Negative. ECG showed old Inferior Wall Myocardial Infarction. 2D Echo revealed RWMA in RCA territory, concentric LVH, Sclerotic aortic valve with mild AR, Fair LV systolic function, EF-54%. CT-Coronary angio-triple vessel disease (Figure-1).
Thallium study showed Small full thickness infarct in basal inferior wall (25 % area of RCA territory) with fair LV function at rest, There is significant stress inducible ischemia in RCA territory as well as in adjoining LCX territory and Diagonal branch territory. There is associated transient LV dilatation and also angina. Myocardial perfusion is normal in LAD territory (Figure-2).
CAG-Right Transradial approach 5Fr Tiger catheter, which revealed LMCA Normal, LAD mid long segment calcific 40-50% lesion, Diagonal-Normal, LCX Non dominant, proximal 90% lesion, OM1-Proximal 70% lesion, RCA proximal total occlusion, distal vessel filling retrogradely (Figure-3). FFR study of LAD was done to rule out any significant disease to decide the need for CABG which showed 0.83 value indicating insignificant lesion even after NTG and IV Adenosine (Figure-4). In view of significant two vessel disease of RCA and Lcx option of PCI with DES was choosen in view of no additional advantage of CABG over PCI strategy.
Procedure:
Procedure performed through Right femoral artery and Right Transradial using 6Fr JR 3.5 guiding catheter through RFA and Tiger catheter through Rt Radial Approach. Simultaneous Rt and Lt coronary injections showed RCA proximal total occlusion with retrograde filling from left collaterals. Initially totally occlusion RCA proximal Lesion was crossed using graded wire escalation strategy.
Tried to cross with 0.014 Fielder XT and gaia-first wire but could not cross, finally crossed with the help of Gaia second wire after multiple manipulations using fine cross microcatheter support. Multiple Predilatations done with 1.25x10mm Tazuna, 2.25x15mm and 2.5x15mm mini trek balloons. Mid RCA stenting did with 2.75x40mm Yukon choice flex stent (DES), Proximal RCA Stenting done with 3.0x12mm Yukon choice flex stent (DES). Post-dilatation did with 3.0x15mm NC Trek balloon (Figure-5). Post-procedure angio view showed well implanted stents with TIMI-III flow without any dissection. Patient was discharged on 4th post procedure day in a stable status, he is under follow-up for the past one and half year without any CV symptoms.
Conclusion:
In a patient with triple vessel disease with CTO of one or two vessels decision of management strategy of Multivessel PCI vs CABG sometimes very difficult but multi modality approach using CT-Angio, Thallium study, FFR and intravascular imaging will be useful in decision making to get the best possible clinical outcomes with low MACE rate. FFR study of borderline LAD was done to choose option between CABG and multivessel PCI, FFR showed no significant LAD. Stress thallium and myocardial viability was done to assess any inducible ischemia and area of viable myocardium in previously infartcted territory.
Thallium study revealed large area of viable myocardium in RCA territory with significant inducible ischemia Hence PCI of CTO of RCA was planned initially considering large dominant RCA. CT-Coronary angio was done prior to PCI to assess length of the totally occluded RCA and to see plaque nature of occluded segment and course of the vessel to manipulate wire to cross CTO.
CT-angio did not show significant calcium of the totally occluded segment, revealed course and length of the CTO segment Hence graded wire escalation strategy was used to cross the CTO segment. If CT-Angio shows significant calcium, highly tortuous course antegrade approach may not be successful and in such circumstances, retrograde technique would be useful. Intravascular imaging (IVUS/OCT) useful in assessing plaque nature and any need for plaque modification strategies, choosing the proper length and diameter of the stent, stent expansion, under expansion, malapposition, detecting edge dissections and any plaque prolapse.
Intravascular imaging also useful in assessing guide wire position whether it s true lumen or false lumen and detects any intramural hematomas which are very difficult to assess with regular angiography. Optimization of the PCI with intravascular imaging is associated with better long term outcomes which is evident in many recently published clinical trials. Multiple imaging modalities and functional assessment with FFR will be very useful in choosing optimal technique in a cost-effective way with minimal procedural complications and better long term outcomes.
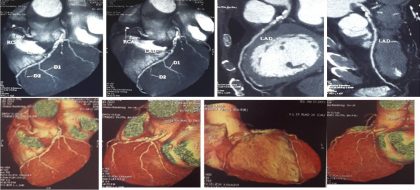 Figure-1: CT-Coronary Angiogram
Figure-1: CT-Coronary Angiogram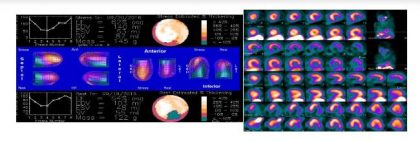 Figure-2: Stress Thallium Study
Figure-2: Stress Thallium Study Figure-3: Coronary Angiogram- LAD mid mild disease, LCX proximal 80% lesion, RCA proximal total occlusion.
Figure-3: Coronary Angiogram- LAD mid mild disease, LCX proximal 80% lesion, RCA proximal total occlusion.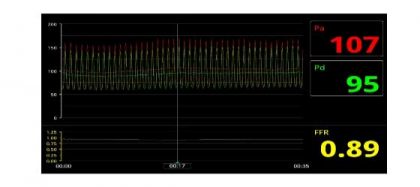 Figure-4: FFR study of LAD-Insignificant leison
Figure-4: FFR study of LAD-Insignificant leison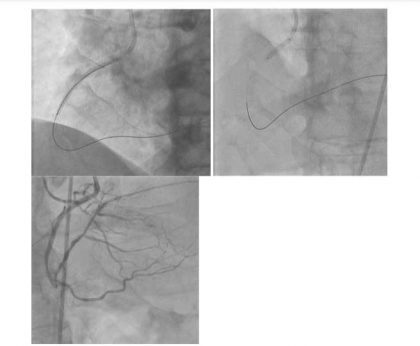 Figure-5: Stenting of RCA
Figure-5: Stenting of RCAThe author, Dr Sridhar Kasturi HOD and Senior Interventional cardiologist at Sunshine hospital paradise Telangana is Presenting on topic Multi-Modality Approach in Managing Triple Vessel Disease at Indialive 2018

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd