- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
MRI guided biopsy improves detection rate in prostate cancer
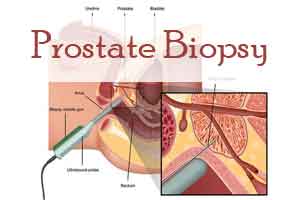
MRI-guided biopsy (MRGB) is an emerging technology with the promise of improving cancer detection rates in prostate cancer, increasing the accuracy of pathological grading, and potentially decreasing the number of biopsy cores taken. Clinically significant cancer was detected in 38% in the MRI-targeted biopsy group, as compared with 26% in the standard-biopsy group, in a recent study
Dr Veeru Kasivisvanathan and his associates conducted multicenter, randomized, noninferiority trial, in 11 countries at 25 centres which included 500 men with a clinical suspicion of prostate cancer who had not undergone biopsy previously to undergo MRI, with or without targeted biopsy, or standard transrectal ultrasonography-guided biopsy. Men in the MRI-targeted biopsy group underwent a targeted biopsy (without standard biopsy cores) if the MRI was suggestive of prostate cancer; men whose MRI results were not suggestive of prostate cancer were not offered biopsy. Standard biopsy was a 10-to-12–core, transrectal ultrasonography-guided biopsy.
The primary outcome was the proportion of men who received a diagnosis of clinically significant cancer. Secondary outcomes included the proportion of men who received a diagnosis of clinically insignificant cancer.
In the MRI-targeted biopsy group, 71 of 252 men (28%) had MRI results that were not suggestive of prostate cancer, so they did not undergo biopsy. Clinically significant cancer was detected in 95 men (38%) in the MRI-targeted biopsy group, as compared with 64 of 248 (26%) in the standard-biopsy group (adjusted difference, 12 percentage points; 95% confidence interval [CI], 4 to 20; P=0.005).
MRI, with or without targeted biopsy, was noninferior to standard biopsy, and the 95% confidence interval indicated the superiority of this strategy over standard biopsy. Fewer men in the MRI-targeted biopsy group than in the standard-biopsy group received a diagnosis of clinically insignificant cancer (adjusted difference, −13 percentage points; 95% CI, −19 to −7; P<0.001).
The research concluded that the use of risk assessment with MRI before biopsy and MRI-targeted biopsy was superior to the diagnostic pathway of standard transrectal ultrasonography in men at clinical risk for prostate cancer who had not undergone biopsy previously.
The study was published in the journal The New England Journal of Medicine
For more reference log on to: https://www.nejm.org/doi/full/10.1056/NEJMoa1801993

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd