- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Management of primary sclerosing cholangitis: BSG Guideline
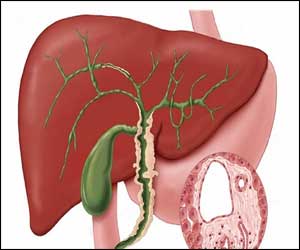
The British Society of Gastroenterology has released guideline on the diagnosis and management of primary sclerosing cholangitis (PSC).
The guidelines, published in the BMJ Journal Gut aims to support general physicians, gastroenterologists and surgeons in managing adults with PSC or those presenting with similar cholangiopathies which may mimic PSC, such as IgG4 sclerosing cholangitis.
PSC is an immune-mediated chronic liver disease characterised by inflammation, fibrosis and destruction of intrahepatic and/or extrahepatic bile ducts leading to cholestasis, bile duct strictures and hepatic fibrosis, which in turn may progress to cirrhosis, portal hypertension and hepatic decompensation.
Key Recommendations:
- Cholestatic liver biochemistry with typical cholangiographic should feature in the absence of other identifiable causes of secondary sclerosing cholangitis is usually sufficient for a diagnosis of PSC.
- MRCP should be the principal imaging modality for the investigation of suspected PSC. ERCP should be reserved for patients with biliary strictures requiring tissue acquisition (eg, cytological brushings) or where therapeutic intervention is indicated.
- Liver biopsy should be normally reserved for possible small duct PSC, assessment of suspected possible overlap variants or instances where the diagnosis is unclear.
- Risk stratification should be carried out on the basis on non-invasive assessment. Clinical scores are an emerging theme but no single method can be recommended at present to predict individual patient prognosis.
- Ursodeoxycholic acid (UDCA) should not be used for the routine treatment of newly diagnosed PSC. For patients already established on UDCA therapy, there may be evidence of harm in patients taking high dose UDCA 28–30 mg/kg/day.
- UDCA should not be used for the prevention of colorectal cancer or cholangiocarcinoma.
- Corticosteroids and immunosuppressants should not be indicated for the treatment of classic PSC. In those patients with additional features of autoimmune hepatitis (AIH) or IgG4-related sclerosing cholangitis (IgG4-SC), corticosteroids may be indicated.
- Endoscopic screening for oesophageal varices should be done in line with international guidelines where there is evidence of cirrhosis and/or portal hypertension.
- Colitis should be sought in all patients with PSC using colonoscopy and colonic biopsies.
- Patients with suspected PSC undergoing ERCP should receive prophylactic antibiotics.
- Non-invasive investigations such as MRCP, dynamic liver MRI and/or contrast CT should be performed in patients who have new or changing symptoms or evolving abnormalities in laboratory investigations.
- Patients with PSC should ordinarily not undergo ERCP until there has been expert multidisciplinary assessment to justify endoscopic intervention.
- In patients undergoing ERCP for dominant strictures, pathological sampling of suspicious strictures is mandatory.
- In patients undergoing ERCP for dominant strictures, biliary dilatation is preferred to the insertion of biliary stents.
- Provision of care should involve a partnership between patients, primary care and hospital-led specialty medicine with consideration made with regard to patient risk assessment, symptom burden and how local services are configured.
- Patients with symptomatic, evolving or complex disease should be referred for expert multidisciplinary assessment. Patients with early, stable disease can be managed in general clinics.
- Patients with PSC meeting inclusion criteria should be offered referral to a centre participating in clinical trials.
- PSC is a well-recognised indication for liver transplantation. Eligibility and referral should be assessed in line with the national guidelines.
- All patients with PSC should have a risk assessment for osteoporosis. Once osteoporosis is detected, treatment and follow-up should be in accordance with national guidelines.
- Poor nutrition and fat-soluble vitamin deficiency are relatively common in advanced PSC and clinicians should have a low threshold for empirical replacement.
- In patients with fatigue, alternative causes should be actively sought and treated.
- Cholestyramine (or similar) should be the first-line medical treatment for pruritus. Rifampicin and naltrexone are second-line treatments.
- An elevated CA19.9 may support a diagnosis of suspected cholangiocarcinoma but has a low diagnostic accuracy. Routine measurement of serum CA19.9 is not recommended for surveillance for cholangiocarcinoma in PSC.
- When a diagnosis of cholangiocarcinoma is clinically suspected, referral for specialist multidisciplinary meeting (MDM) review is essential.
- Where cholangiocarcinoma is suspected, contrast-enhanced, cross-sectional imaging remains the initial preferred investigation for diagnosis and staging.
- An annual ultrasound scan of the gallbladder should be performed in patients with PSC. If polyps are identified, treatment should be directed by specialist hepatopancreaticobiliary (HPB) MDM.
- Patients with PSC who have coexistent colonic inflammatory bowel disease (IBD) should have annual colonoscopic surveillance from the time of diagnosis of colitis in line with the BSG guidelines.
- In the presence of cirrhosis, hepatocellular carcinoma surveillance should be carried out in accordance with international guidelines.
- Because pregnancy in cirrhotic patients carries a higher risk of maternal and fetal complications, patients should have preconception counselling and specialist monitoring.
- Patients with PSC should be encouraged to participate in patient support groups.
For complete access to the guideline follow the link: http://dx.doi.org/10.1136/gutjnl-2018-317993
bile ductsBMJcholangiocarcinomacholestasischolestyraminechronic liver diseaseCirrhosisCorticosteroidsGallbladderHepatocellular CarcinomaIgG4 sclerosing cholangitisimmunosuppressantsinflammatory bowel diseaseliver biopsymagnetic resonance cholangiopancreatographynaltrexoneportal hypertensionprimary sclerosing cholangitisrifampicinursodeoxycholic acid
Next Story
NO DATA FOUND

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd