- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
Management of adult pancreatic injuries: Guideline
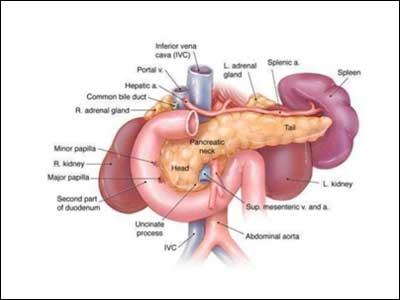
Traumatic injury to the pancreas is rare but is associated with significant morbidity and mortality, including fistula, sepsis, and death. There are currently no practice management guidelines for the medical and surgical management of traumatic pancreatic injuries.
U.S. Department of Health and Human Services,Eastern Association for the Surgery of Trauma have issued the Management of adult pancreatic injuries: a practice management guideline
Following are the major recommendations :
Treatment of Low-Grade Injury Diagnosed by Computed Tomography (CT) (Patient, Intervention, Comparators, Outcome [PICO] 1)
For adult patients with grade I/II injuries to the pancreas identified by CT scan, should operative intervention or nonoperative management be performed?
Recommendation
The guideline authors conditionally recommend nonoperative management for grade I/II pancreatic injuries diagnosed by CT scan. Nonoperative management appears to have low morbidity. If the pancreatic duct is not definitively intact, it seems reasonable to further evaluate the duct with additional tests, such as endoscopic retrograde cholangiopancreatography (ERCP) or magnetic resonance cholangiopancreatography (MRCP), because this may change the grade of the injury and therefore the recommended treatment plan.
Treatment of High-Grade Injury Diagnosed by CT (PICO 2)
For adult patients with grade III/IV injuries to the pancreas identified on CT scan, should operative intervention or nonoperative management be performed?
Recommendation
The guideline authors conditionally recommend operative management for grade III/IV pancreatic injuries diagnosed by CT scan. Although there was no statistically significant difference between groups for any single outcome, the guideline group feels that there is a cumulative trend toward increased morbidity after nonoperative management. Treatment failures after nonoperative management occur regularly, and treatment delays likely contribute to morbid complications and death.
Operative Management of Low-Grade Injury (PICO 3)
For adults undergoing an operation who are intraoperatively found to have a grade I/II pancreas injury, should resectional or nonresectional management be performed?
Recommendation
The guideline authors conditionally recommend nonresectional management for operative management of grade I/II pancreatic injuries. Pooled data analysis suggests that mortality from pancreas-related causes is generally low in this population and that there were significantly more intra-abdominal abscesses in the resection group.
Operative Management of High-Grade Injury (PICO 4)
For adults already undergoing an operation who are intraoperatively found to have a grade III/IV pancreas injury, should resection or nonresection be performed?
Recommendation
The guideline authors conditionally recommend resection for operative management of grade III/IV pancreatic injuries. Complications are frequent in both groups. In the pooled analysis, fistula development was associated with nonresection strategies. Pancreas-related mortality was higher in the nonresection group, but this finding was potentially confounded by incomplete mortality reporting and bias. Due to the very low quality of available data, this is a conditional recommendation.
Treatment of Grade V Injury (PICO 5)
For adults with total destruction of the head of the pancreas (grade V), should pancreaticoduodenectomy or surgical treatment other than pancreaticoduodenectomy be performed?
Recommendation
No recommendation is given. The literature on this topic is limited and dated. Surgical and resuscitation strategies have evolved significantly to include damage control procedures and early balanced resuscitations, making the guideline authors' ability to interpret the available literature limited. Grade V injury to the pancreas is extremely morbid, and the intraoperative and immediate postoperative rate of death is high.
Routine Postoperative Fistula Prophylaxis with Octreotide (PICO 6)
For adult patients who have undergone an operation for pancreatic trauma, should routine octreotide prophylaxis or no octreotide be used?
Recommendation
The guideline authors conditionally recommend against the routine use of octreotide for postoperative prophylaxis related to traumatic pancreatic injuries to prevent fistula. Data are limited, but pooled data show no difference in outcomes between groups. The subcommittee concluded that the less invasive (no medication) strategy would be preferable with no difference in outcomes.
Routine Splenectomy with Distal Pancreatectomy (PICO 7)
For adults undergoing a distal pancreatectomy for trauma, should routine splenectomy or splenic preservation be performed?
Recommendation
No recommendation is given. Existing data do not support either treatment modality, although splenic preservation was only considered for stable patients. If either the stability of the patient or the surgeon's ability to safely preserve the spleen is in doubt, a distal pancreatectomy with splenectomy is a reasonable choice.
Read the full guideline click on the link :
Ho VP, Patel NJ, Bokhari F, Madbak FG, Hambley JE, Yon JR, Robinson BR, Nagy K, Armen SB, Kingsley S, Gupta S, Starr FL, Moore HR III, Oliphant UJ, Haut ER, Como JJ. Management of adult pancreatic injuries: a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2017 Jan;82(1):185-99. [58 references] PubMed

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd