- Home
- Editorial
- News
- Practice Guidelines
- Anesthesiology Guidelines
- Cancer Guidelines
- Cardiac Sciences Guidelines
- Critical Care Guidelines
- Dentistry Guidelines
- Dermatology Guidelines
- Diabetes and Endo Guidelines
- Diagnostics Guidelines
- ENT Guidelines
- Featured Practice Guidelines
- Gastroenterology Guidelines
- Geriatrics Guidelines
- Medicine Guidelines
- Nephrology Guidelines
- Neurosciences Guidelines
- Obs and Gynae Guidelines
- Ophthalmology Guidelines
- Orthopaedics Guidelines
- Paediatrics Guidelines
- Psychiatry Guidelines
- Pulmonology Guidelines
- Radiology Guidelines
- Surgery Guidelines
- Urology Guidelines
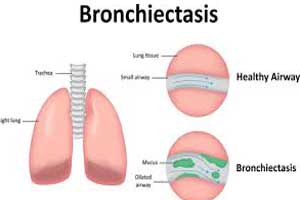
Management of acute exacerbation of bronchiectasis: NICE 2018 Guidance
NICE (National Institute for Health and Care Excellence) has released a guidance document, on antimicrobial prescribing strategy for managing and preventing acute exacerbations of bronchiectasis. It aims to optimise antibiotic use and reduce antibiotic resistance.
This guideline includes recommendations on:-
• treatment
• reassessment
• referral and seeking specialist advice
• choice of antibiotic for treatment
• prevention
The key recommendations are:-
A. Antibiotics - treatment
When choosing antibiotics, take account of:
• the severity of symptoms
• previous exacerbations, hospitalisations, and risk of complications
• previous sputum culture and susceptibility results
• Give oral antibiotics first line if possible
B. Antibiotics – prophylaxis
- Only start a trial of antibiotic prophylaxis on specialist advice
- When considering antibiotic prophylaxis, discuss the possible benefits (reduced exacerbations), harms (increased antimicrobial resistance, adverse effects, and interactions with other medicines) and the need for regular review
C. Reassessment
Reassess people with an acute exacerbation of bronchiectasis if their symptoms worsen rapidly or significantly at any time, taking account of:
- other possible diagnoses, such as pneumonia
- any symptoms or signs suggesting a more serious illness or condition, such as cardiorespiratory failure or sepsis
- previous antibiotic use, which may have led to resistant bacteria
D. Referral and seeking specialist advice
Seek specialist advice for people with an acute exacerbation of bronchiectasis if they:
- have symptoms that are not improving with repeated courses of antibiotic treatment or
- have bacteria that are resistant to oral antibiotics or
- follow table 1 for adults aged 18 years and over
follow table 2 for children and young people under 18 years.cannot take oral medicines
Choice of antibiotic for treating the acute exacerbation of bronchiectasis
1. When prescribing antibiotic treatment for an acute exacerbation of bronchiectasis:
- Give oral antibiotics first line if the person can take oral medicines, and the severity of their condition does not require intravenous antibiotics.
- Review intravenous antibiotics by 48 hours and consider stepping down to oral antibiotics where possible.
Table 1 Antibiotics for adults aged 18 years and over
Antibiotic Dosage and course length First-choice oral antibiotics for empirical treatment in the absence of current susceptibility data (guided by most recent sputum culture and susceptibilities where possible) Amoxicillin3 500 mg three times a day for 7 to 14 days Doxycycline 200 mg on first day, then 100 mg once a day for a 7- to 14‑day course Clarithromycin 500 mg twice a day for 7 to 14 days Alternative choice oral antibiotics (if the person at higher risk of treatment failure ) for empirical treatment in the absence of current susceptibility data (guided by most recent sputum culture and susceptibilities where possible) Co-amoxiclav 500/125 mg three times a day for 7 to 14 days Levofloxacin6 500 mg once or twice a day for 7 to 14 days First-choice intravenous antibiotics (if unable to take oral antibiotics or severely unwell) for empirical treatment in the absence of current susceptibility data (guided by most recent sputum culture and susceptibilities where possible) 7 Co-amoxiclav 1.2 g three times a day Piperacillin with tazobactam 4.5 g three times a day, increased if necessary to 4.5 g four times a day Levofloxacin6 500 mg once or twice a day When current susceptibility data available, choose antibiotics accordingly Consult local microbiologist as needed 1 See the British national formulary (BNF) for appropriate use and dosing in specific populations, for example, hepatic impairment, renal impairment, pregnancy and breastfeeding, and administering intravenous antibiotics.
2 When a person is receiving antibiotic prophylaxis, treatment should be with an antibiotic from a different class.
3 Amoxicillin is the preferred choice for women who are pregnant.
4 Course length based on an assessment of the severity of bronchiectasis, exacerbation history, severity of exacerbation symptoms, previous culture and susceptibility results, and response to treatment.
5 People who may be at higher risk of treatment failure include people who have had repeated courses of antibiotics, a previous sputum culture with resistant or atypical bacteria, or a higher risk of developing complications.6 The European Medicines Agency's Pharmacovigilance Risk Assessment Committee has recommended restricting the use of fluoroquinolone antibiotics following a review of disabling and potentially long-lasting side effects mainly involving muscles, tendons, bones and the nervous system. This includes a recommendation not to use them for mild or moderately severe infections unless other antibiotics cannot be used (press release October 2018).
7 Review intravenous antibiotics by 48 hours and consider stepping down to oral antibiotics where possible for a total antibiotic course of 7 to 14 days.
Table 2 Antibiotics for children and young people under 18 years
Antibiotic Dosage and course length First-choice oral antibiotics for empirical treatment in the absence of current susceptibility data (guided by most recent sputum culture and susceptibilities where possible) Amoxicillin4 1 to 11 months, 125 mg three times a day for 7 to 14 days
1 to 4 years, 250 mg three times a day for 7 to 14 days
5 to 17 years, 500 mg three times a day for 7 to 14 daysClarithromycin 1 month to 11 years:
Under 8 kg, 7.5 mg/kg twice a day for 7 to 14 days
8 to 11 kg, 62.5 mg twice a day for 7 to 14 days
12 to 19 kg, 125 mg twice a day for 7 to 14 days
20 to 29 kg, 187.5 mg twice a day for 7 to 14 days
30 to 40 kg, 250 mg twice a day for 7 to 14 days
or
12 to 17 years, 250 mg to 500 mg twice a day for 7 to 14 daysDoxycycline 12 to 17 years, 200 mg on first day, then 100 mg once a day for a 7- to 14‑day course in total Alternative choice oral antibiotics (if person at higher risk of treatment failure ) for empirical treatment in the absence of current susceptibility data (guided by most recent sputum culture and susceptibilities where possible) Co-amoxiclav 1 to 11 months, 0.25 ml/kg of 125/31 suspension three times a day for 7 to 14 days
1 to 5 years, 5 ml of 125/31 suspension three times a day or 0.25 ml/kg of 125/31 suspension three times a day for 7 to 14 days
6 to 11 years, 5 ml of 250/62 suspension three times a day or 0.15 ml/kg of 250/62 suspension three times a day for 7 to 14 days
12 to 17 years, 250/125 mg three times a day or 500/125 mg three times a day for 7 to 14 daysCiprofloxacin (on specialist advice) 1 to 17 years, 20 mg/kg twice daily (maximum 750 mg per dose) for 7 to 14 days5 First-choice intravenous antibiotics (if unable to take oral antibiotics or severely unwell) for empirical treatment in the absence of current susceptibility data (guided by most recent sputum culture and susceptibilities where possible) Co-amoxiclav 1 to 2 months, 30 mg/kg twice a day
3 months to 17 years, 30 mg/kg three times a day (maximum 1.2 g three times a day)Piperacillin with tazobactam 1 month to 11 years, 90 mg/kg three or four times a day (maximum per dose 4.5 g four times a day)
12 to 17 years, 4.5 g three times a day, increased if necessary to 4.5 g four times a dayCiprofloxacin (on specialist advice)7 1 to 17 years, 10 mg/kg three times a day (maximum 400 mg per dose) When current susceptibility data available, choose antibiotics accordingly Consult local microbiologist as needed 1 See BNF for children for appropriate use and dosing in specific populations, for example, hepatic impairment and renal impairment, and administering intravenous antibiotics.
2 When a person is receiving antibiotic prophylaxis, treatment should be with an antibiotic from a different class.
3 The age bands apply to children of average size and, in practice, the prescriber will use the age bands in conjunction with other factors such as the severity of the condition and the child's size in relation to the average size of children of the same age.
4 Amoxicillin is the preferred choice in young women who are pregnant.
5 Course length based on an assessment of the severity of bronchiectasis, exacerbation history, severity of exacerbation symptoms, previous culture and susceptibility results, and response to treatment.
6 People who may be at higher risk of treatment failure include people who have had repeated courses of antibiotics, a previous sputum culture with resistant or atypical bacteria, or a higher risk of developing complications.
7 The European Medicines Agency's Pharmacovigilance Risk Assessment Committee has recommended restricting the use of fluoroquinolone antibiotics following a review of disabling and potentially long-lasting side effects mainly involving muscles, tendons, bones and the nervous system. This includes a recommendation not to use them for mild or moderately severe infections unless other antibiotics cannot be used (press release October 2018).
8 Review intravenous antibiotics by 48 hours and consider stepping down to oral antibiotics where possible for a total antibiotic course of 7 to 14 days.
For more details click on the link: www.nice.org

Disclaimer: This site is primarily intended for healthcare professionals. Any content/information on this website does not replace the advice of medical and/or health professionals and should not be construed as medical/diagnostic advice/endorsement or prescription. Use of this site is subject to our terms of use, privacy policy, advertisement policy. © 2020 Minerva Medical Treatment Pvt Ltd